A Case of Immunoglobulin Responsive Medically Refractory Epilepsy Secondary to GABA B Receptor Antibody Encephalitis With Extra-Limbic MRI FLAIR Lesions
Abstract number :
1.448
Submission category :
18. Case Studies
Year :
2018
Submission ID :
500411
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Keerthana Akkineni, Houston Methodist Neurological Institute; Hina Aslam, Houston Methodist Neurological Institute; Amit Verma, Houston Methodist Neurological Institute; Brooke McQueen, Houston Methodist Neurological Institute; and Sheetal Shroff, Houston
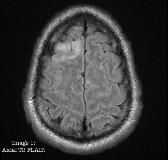
Rationale: Two to six percent of patients with generalized clonic status epilepticus are a result of autoimmune or paraneoplastic encephalitis1. We present a case of new adult onset medically refractory epilepsy secondary GABA B receptor Ab encephalitis with good response to immunotherapy and extra-limbic FLAIR lesions on MRI. Methods: 52-year-old man was admitted to the neurointensive care unit with new onset status epilepticus with bilateral frontotemporal seizure onset recorded on EEG. Initial MRI brain w contrast was unremarkable. Repeat MRI brain day-13 revealed FLAIR changes in both temporal (Image 2) and right frontal lobes (Image 1). CSF showed lymphocytic leukocytosis (WBC 37, 84% lymphocytes) with elevated IgG synthesis rate. CSF cultures & viral PCRs were negative.Over the course of ICU stay, he was treated with levetiracetam, lacosamide, oxcarbazepine, valproic acid, midazolam drip, topiramate, perampanel, tiagabine, phenytoin and IV methylprednisolone 1000 mg daily for 5 days. EEG continued to show electrographic seizures.On day 18, serum autoimmune encephalitis panel was positive for GABA B receptor ab (1:512). 4 doses of 0.6 mg/kg IVIG was given cautiously as he developed a pulmonary embolism. After 2 days of IVIG, there was resolution of electrographic seizures. A second course of IV methylprednisolone 1000 mg daily for 5 days was also given. His mental status has improved and he became communicative. His CT chest revealed a small lung nodule for which further work up is planned when stable. Results: GABA B receptor ab encephalitis presents with early seizures and has a higher association with cancer2. Typical imaging features include hyperintensity in medial temporal lobes on MRI FLAIR though extra-limbic lesions is reported2. In a case series of 15 patients, 10 had evidence of mesial temporal lobe involvement, 1 of corpus callosum and 4 normal MRI3. Similarly, in our patient, initial MRI was unremarkable, however repeat imaging revealed FLAIR hyperintensities not only in both medial temporal lobes (Image 2) but also the right frontal lobe (Image 1). Management includes evaluation for underlying and first-line immunotherapies including high dose steroids/ IVIG/ plasma exchange4. If unresponsive, then cyclophosphamide/ rituximab can be considered (2nd line). According to a case series of 15 patients with GABA B receptor ab encephalitis, 60-70% showed response to immune and tumor therapy3. Similarly, in a case series of 577 patients with NMDAR encephalitis, early treatment with immunotherapy was an independent predictor of good outcome. Those who didn’t respond to first-line therapy responded to second-line and both had reduced number of relapses.4 Conclusions: GABA B receptor ab encephalitis can present with extra-limbic MRI FLAIR changes & has a higher association with small cell lung cancer and pulmonary neuroendocrine tumors2. Evaluation for occult malignancy should be sought with early removal of tumor. The role of early immunotherapy for the acute management of patients with medically refractory status needs further study.References1. Spatola M, et al. Status epilepticus of inflammatory etiology: a cohort study. Neurology. 2015 Aug 4;85(5):464-470.2. Kelley BP, et al. Autoimmune encephalitis: pathophysiology and imaging review of an overlooked diagnosis. Am J Neuroradiol. 2017;38(6):1070-1078.3. Lancaster E, et al. Antibodies to the GABA(B) receptor in limbic encephalitis with seizures: case series and characterisation of the antigen. Lancet Neurol. 2010;9:67–76.4. Titulaer MJ, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 2013;12:157–165. Funding: None
.tmb-.jpg?Culture=en&sfvrsn=e6ad74f2_0)