A Learning Healthcare System for Epilepsy: Organization and Management
Abstract number :
1.412
Submission category :
13. Health Services (Delivery of Care, Access to Care, Health Care Models)
Year :
2018
Submission ID :
502524
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Zachary Grinspan, Weill Cornell Medicine; Natasha Basma, Weill Cornell Medicine; Jeffrey Buchhalter, Mayo Clinic; Anup D. Patel, Nationwide Children's Hospital; Anne T. Berg, Ann & Robert H. Lurie Children's Hospital of Chicago; Renee Shellhaas, C.S. Mott
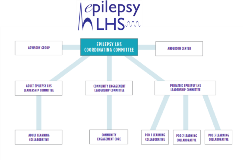
Rationale: A learning healthcare system (LHS) collects administrative and clinical data entered at the point of care, aggregates and analyzes the data across multiple sites, then regularly reports findings back to sites to continuously improve care. For example, the pediatric inflammatory bowel disease LHS improved remission rates from 50% to 80% in 10 years without new medications (ImproveCareNow). “Co-production” of improvement among patients/families, clinicians, and researchers is a core component of an effective LHS, and ensures alignment across multiple stakeholders.Creating an LHS for epilepsy poses novel opportunities and challenges to LHS design for multiple reasons, including (a) the close relationship between the pediatric and adult epilepsy communities, (b) the large number of individuals (3.4 million Americans with epilepsy), (c) heterogeneity of the epilepsies, and (d) diversity of advocacy groups for common and rare epilepsies. We propose and field test an organization and management approach to develop an LHS for epilepsy. Methods: In 2017 & 2018, over multiple phone calls, in-person meetings, and email correspondence, the authors discussed and operationalized an approach to construct a learning healthcare system for epilepsy. Topics included the vision and goals of an LHS in epilepsy, key drivers of success, organizational structure and governance, patient and family involvement, informatics & technology, business model and sustainability, ethics, legal agreements, consulting / coaching agreements, metrics for success, and opportunities for alignment with other organizations. Results: The vision of an epilepsy learning health system is that all people with epilepsy are seizure free and living at their highest quality of life. The organizational structure of the Epilepsy LHS consists of three coordinated but autonomous cores: Pediatrics, Adult, and Community Engagement. The Pediatric Epilepsy Learning Health System (PELHS) has recruited 18 sites and leads three monthly phone calls ("pod calls") to establish legal, ethical, and technical infrastructure. The data coordinating center (DCC) for the PELHS has piloted registry questions and a reporting pipeline using open source technology. A central IRB protocol and data use agreements with the DCC are executed at 10 pediatric sites. The Adult Epilepsy Core has established working groups focused on developing specific key drivers of improved outcomes, including screening and treatment for psychiatric comorbidities, counseling for reproductive planning, and referral and evaluation for surgery and other comprehensive epilepsy care options. The Community Engagement Core (including the Rare Epilepsy Network partners and patients/family representative with more common epilepsies) has held in person and teleconference meetings to develop patient/family priorities for the LHS, explore methods of connecting with empathy, and learn more about quality improvement methodology and patient/family “co-production” with researchers and clinicians. Conclusions: An epilepsy learning healthcare system is feasible and under active construction. Further work is needed to measure its effect on outcomes. Funding: Epilepsy Foundation