Acute Encephalopathy With Biphasic Seizures and Late Reduced Diffusion Associated With Adenoviral Pneumonia
Abstract number :
2.436
Submission category :
18. Case Studies
Year :
2018
Submission ID :
501670
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Bo Lyun Lee, Busan Paik Hospital, Inje University College of Medicine; Keun Soo Lee, Busan Paik Hospital, Inje University College of Medicine; and Ji Yeon Lee, Busan Paik Hospital, Inje University College of Medicine
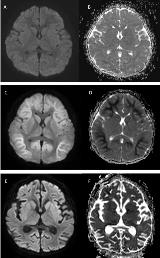
Rationale: Acute encephalopathy with biphasic seizures and late reduced diffusion (AESD) is a subtype of acute encephalopathy described in a cohort of Japanese children. It is characterized clinically by biphasic seizures and late reduced subcortical diffusion on magnetic resonance imaging (MRI). Reports of AESD involving other ethnic groups are rare, as are those with a preceding adenovirus infection. We report the first Korean case of AESD in association with preceding adenoviral infection. Methods: We present clinical, electroencephalographic and radiologic features of our rare case. Results: A previously healthy 3-year-old Korean girl presented with statue epilepticus that started with focal impaired awareness with upward eye deviation following a 5-day prodromal illness consisting of fever, cough, sputum production, and rhinorrhea. Her seizures were refractory to typical doses of benzodiazepines but were subsequently controlled with a bolus of intravenous phenobarbital. Her chest radiograph showed pneumonic consolidation of the right lower lung field. Blood, urine, and CSF cultures showed no growth, and CSF polymerase chain reaction (PCR) for enterovirus, herpes simplex virus type 1 and 2, varicella zoster virus, cytomegalovirus, measles, HHV-6, and adenovirus was negative. However, multiplex real-time reverse transcriptase PCR assay for respiratory viruses from a nasopharyngeal aspirate was positive for human adenovirus. Initial brain MRI with diffusion-weighted imaging (DWI) and electroencephalography (EEG) showed no abnormality on day 3 of hospitalization (Figure 1A & 1B). After 5 days, she developed a second cluster of seizures followed by altered consciousness, aphasia, stereotypic movement, and developmental regression. Her seizure was controlled with levetiracetam. Her brain MRI showed symmetrical and extensive restricted diffusion in the subcortical white matter, which finally resulted in global brain atrophy, consistent with AESD (Figures 1C & 1D). Approximately 1 month later, she regained her gross motor functions. However, her brain MRI showed diffused atrophic changes involving both cerebral hemispheres (Figure 1E & 1F). One year later, she still showed psychomotor developmental regression and focal epilepsy, with diffused parenchymal atrophy without any interval change on brain MRI. Conclusions: We report what is, to our knowledge, the first case of a Korean child presenting with AESD preceded by adenoviral pneumonia. However, many cases with AESD might be missed because MRI abnormality is not seen for a few days. The diagnosis of AESD is based on the presence of biphasic seizures, and distinctive imaging features. Brain MRI with DWI is an essential tool to detect this type of encephalopathy in a patient with febrile status epilepticus who is showing repetitive seizures or neurologic deterioration. Therefore, pediatric neurologists should be aware of the clinicoradiologic features of acute encephalopathy and perform brain MRI aggressively in patients suspected of having AESD, to detect the dynamic MRI changes. Funding: None