Aura as a Predictor of Outcome Following Epilepsy Surgery
Abstract number :
3.322
Submission category :
9. Surgery / 9A. Adult
Year :
2018
Submission ID :
497639
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Scott Grossman, New York University Comprehensive Epilepsy Center; Jacqueline A. French, New York University Comprehensive Epilepsy Center; and Patricia Dugan, NYU Langone School of Medicine
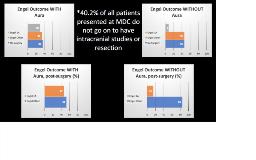
Rationale: Auras are an excellent clinical indicator of possible location of the seizure onset zone (SOZ), because they are the first symptom to appear in the course of a seizure. The goal of resective epilepsy surgery remains seizure freedom and presurgical evaluation aims to identify the SOZ. Several studies have investigated pre-surgical value of aura in predicting seizure outcome in temporal lobe epilepsy but similar studies have not been broadly performed in a mixed population of both temporal and extra-temporal epilepsy. This study aims to assess the relationship of defined aura with surgical outcome. Methods: Data on all patients at the NYU Comprehensive Epilepsy Center who presented for evaluation at the pre-surgical Multidisciplinary Conference (MDC) were obtained from a database that organizes the epilepsy surgery program. This proof of concept study investigated all patients presenting in calendar year 2011 (103). Inclusion criteria for our study included subject age greater than 12. Exclusion criteria included known developmental delay, IQ less than 70 per neuropsychology testing and co-occurrence of NES. Outcome data of interest included localization obtained at MDC, localization of intracranial EEG, as well as presence and semiology of self-reported aura. Finally, through chart review, outcome data using the Engel Extended Outcome Scale was adjudicated by study authors 24 months after time of MDC presentation. Results: Of 103 patients presented in 2011 MDC, 87 met criteria for inclusion in our study. Of this group, 50 patients (57%) reported aura phenomenon on intake at time of MDC presentation and 37 (43%) reported no aura. Of those patients who reported aura 32 (64%) proceeded to resective surgery. Of those proceeding to surgery, 15 (47%) achieved Engel 1A outcome at two years post-surgical follow up. Of patients who denied aura at time of MDC presentation, 20 (54%) proceeded to resective surgery. 3 (15%) achieved Engel 1A outcome at two years post-surgical follow up. The overall rate of non-progression to surgery, 40.2%, is consistent with prior cohort studies using the NYU MDC. Conclusions: In our preliminary study, individuals who reported aura at time of MDC presentation and proceeded to resective surgery were more likely to achieve Engel 1A outcome than patients without aura. This finding needs confirmation from a larger cohort. If confirmed, this could be useful for further clarifying the patient populations that should be referred for pre-surgical workup from a community setting. Scales such as the Epilepsy Surgery Grading Scale (ESGS) could be refined to include data on presence or absence of aura. Funding: No sources of funding