Automated Pre-surgical Localization Softwares: Are They Reliable?
Abstract number :
1.150
Submission category :
3. Neurophysiology / 3C. Other Clinical EEG
Year :
2018
Submission ID :
495711
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Ushtar Amin, University of South Florida; Arathi Nandyala, University of South Florida; Stephanie MacIver, University of South Florida; and Selim Benbadis, University of South Florida
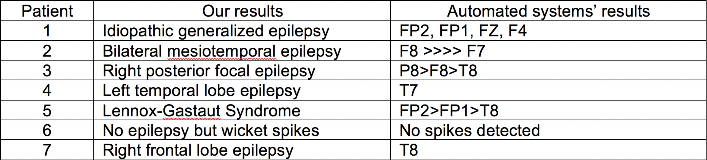
Rationale: Several automated and semi-automated localization softwares are available for the purpose of epilepsy surgery. “Epilog Preop” is an automated process for localization of the seizure focus for the purpose of epilepsy surgery. The claim as advertised is as follows: “Preoperative EEG analysis in epilepsy patients is a time-consuming and labor-intensive process. This often leads to analysis backlogs. Epilog automates the analysis of preoperative EEG data and provides the results in a concise report and 3D viewer with clear visualization for preoperative evaluation.” It is FDA-approved. Our objective was to test it with selected cases of a typical level-4 (surgical) center. Methods: For all patients, automated EEG analysis was performed by Epilog (Epilog co, New York, USA). The automated analysis consisted of spike detection and subsequent EEG source imaging using a patient specific head model constructed from the patient's MRI. In five out of seven patients, a template head model was used because the patients’ MRIs did not meet the company’s requirements. The results of the automated analysis were concisely bundled in an Epilog PreOp report and sent to the treating physician for interpretation. Concordance with the patient's diagnosis was investigated. We selected 7 well-defined cases, diagnosed with a complete non-invasive evaluation, including EEG-video monitoring and imaging. Cases were selected to represent various clinical scenarios, and were as follows (one case each): Clear unilateral mesiotemporal lobe epilepsy; Bitemporal epilepsy; Right posterior hemisphere epilepsy, Idiopathic generalized epilepsy; Lennox-Gastaut syndrome; Right frontal lobe epilepsy; No epilepsy with normal EEG and wicket spikes. Results: See attached table. Conclusions: The software did not “get tricked” and did not incorrectly detect wickets or benign sharp transients as epileptic discharges.It identifies generalized epilepsy as “bi-frontal.” This is understandable since generalized discharges (IGE and LGS type) are usually maximum frontal, but could be misinterpreted as frontal lobe epilepsy.For focal epilepsies, the localization was accurate, but this only applies to interictal discharges, which are of course only one part of the localization process for the purpose of resective surgery.It is unclear if the software really saves time, and whom it would benefit. It is unclear if the software adds anything that wasn't already known about the location of interictal discharges.One potential danger is neurologists relying too much on technology, in a way similar to over-reliance on automated spike detection. Like any tool, it must be interpreted by epileptologists experienced in epilepsy surgery, and in the context of the entire clinical picture.Overall, this may be of value once it is established that the patient has a focal epilepsy. The next version of this software will analyze ictal discharges and should be tested in a similar fashion. Funding: None