Awake Stereotactic Laser Ablation of Focal Cortical Dysplasia with Visual Field Mapping
Abstract number :
3.336
Submission category :
Late Breakers
Year :
2013
Submission ID :
1867038
Source :
www.aesnet.org
Presentation date :
12/7/2013 12:00:00 AM
Published date :
Dec 5, 2013, 06:00 AM
Authors :
D. Xu, S. L. Kalb, S. Chung, A. Shetty, K. Smith
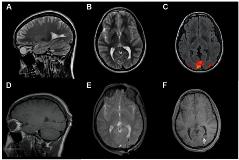
Rationale: Focal cortical dysplasia (FCD) is a significant cause of medically refractory epilepsy but surgical therapy is often limited due to location in eloquent regions. Laser induced thermal therapy (LITT) is a minimally invasive ablative procedure that allows real time visualization of target damage through intraoperative MRI. We report further precision usage of LITT in a patient with medical intractable epilepsy due to FCD in the primary visual cortex through awake LITT with active visual field testing.Methods: The patient is a 17 year old male who at 10 years of age presented with focal visual seizures and multiple episodes of secondary generalization. Subsequent evaluation with continuous EEG localized his seizure activity to the left occipital lobe where follow-up MRI revealed an area of grey matter heterotopia and FCD within the primary visual cortex. Given the eloquent location of this lesion, a minimally invasive approach through LITT was felt as the safest therapeutic option. We chose the FDA-cleared surgical laser ablation system, Visualase (Visualase, Inc., Houston, TX) to be employed. This system relies on a cooled laser catheter (1.6mm in diameter) mounted on a twist hole platform with a 1 cm treatment tip. Preoperatively, a 3T functional MRI study mapping the patient s active visual cortex was fused to a T2-weighted volumetric imaging study for purposes of surgical planning. A suitable trajectory for the ablation catheter was mapped. Intraoperatively, this trajectory was utilized to introduce the LITT ablation (Figure 1). The patient was then moved into a 3.0-T GE Signa EXCITE MRI scanner and kept awake. Magnetic resonance temperature imaging was then accomplished using a fast gradient echo sequence (multi-planar) field of view. After a test dose of 4.5 W for 20-45 seconds to confirm applicator position, two doses of 12W for 120 seconds were used to ablate the foci. Safety limits (50C) were placed near the margins outlined by the patient s pre-operative functional MRI. The patient remained awake during the ablation and visual field tests were done before and after each ablation cycle to verify specificity of treatment.Results: Intraoperative MRI monitoring of the patient s ablation showed full coverage of the targeted lesion without infringement of temperature safety limits along the patient s mapper visual cortex (Figure 2). Similarly, awake visual field testing showed no deficits. The patient tolerated the procedure well without complication and was discharged the following day. On outpatient follow-up he has remained seizure free for 3 months.Conclusions: LITT is a minimally invasive ablative technique that offers several practical advantages over conventional open cranial surgery and radiotherapy for the treatment of epileptogenic foci. Due to its minimally invasive approach, feedback control with MR thermal monitoring, as well as our demonstrated capacity to perform this procedure awake with neurologic monitoring and mapping, LITT remains a substantial option for the treatment of deep seated lesions or those within eloquent regions.