Case of 'Pseudo'-Juvenile Myoclonic Epilepsy Associated with CHD2 Gene Mutation
Abstract number :
1.199
Submission category :
4. Clinical Epilepsy / 4A. Classification and Syndromes
Year :
2018
Submission ID :
501054
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Neeraj Singh, Albany Medical Center and Anthony L. Ritaccio, Albany Medical College
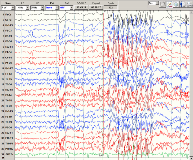
Rationale: To describe a patient with clinical and electroencephalographic (EEG) features commonly associated with juvenile myoclonic epilepsy (JME) in the setting of a rare genetic mutation. Methods: A 12-year-old boy with pervasive developmental delay and no family history of epilepsy was evaluated in our epilepsy clinic after two discrete episodes of witnessed convulsions. Despite being started on lamotrigine, he continued to have events described as twitching of either arm, often out of sleep, which would sometimes generalize. Routine scalp EEG revealed abundant, high-amplitude 4 Hz generalized spike-and-wave and polyspike-and-wave discharges. Results: A 48-hour long-term video EEG subsequently captured two electroclinical seizure semiologies. One was limited to upper extremity myoclonus synchronized with a 5-Hz generalized spike-and-wave burst, as seen in the figure. The other involved upper extremity myoclonus with shifting laterality evolving into a generalized convulsion, synchronized with 5-Hz generalized spike-and-wave activity prior to electrical generalization. Given the patient's developmental delay and seizures, genetic testing was performed and revealed a de novo chromodomain helicase DNA-binding protein 2 (CHD2) gene mutation. Conclusions: This patient's epilepsy initially appeared to meet common criteria for JME, given the age of seizure onset, predominance of myoclonic jerks, high-frequency generalized spike-and-wave activity, and a recorded myoclonic-tonic-clonic seizure. However, JME has not been described to have an association with pervasive developmental delay or CHD2 mutations. Instead, JME has been associated mostly with mutations in the genes for the gamma-aminobutyric acid type A receptor alpha 1 submit (GABRA1) and the EF-hand domain containing protein 1 (EFHC1). De novo CHD2 mutations have established associations with Lennox-Gastaut, Dravet, and Jeavons syndromes, and is thought to show incomplete penetrance or variable expressivity. This presentation of a “pseudo”-JME case represents a less frequently encountered genetic epilepsy that may share a common clinical phenotype. Ultimately, this may be the determinant of our patient’s drug resistance. Funding: Not applicable