Changes in Depression and Anxiety After Stereotactic Laser Amygdalohippocampectomy for Temporal Lobe Epilepsy
Abstract number :
1.373
Submission category :
11. Behavior/Neuropsychology/Language / 11A. Adult
Year :
2018
Submission ID :
498075
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Karanbir S. Padda, Weill Cornell Medicine, New York-Presbyterian Hospital; Robert E. Gross, Emory University School of Medicine; Jon T. Willie, Emory University; Ioannis Karakis, Emory University School of Medicine; Ekaterina Staikova, Emory University Sc
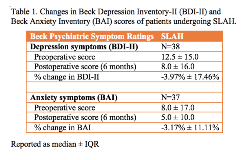
Rationale: Stereotactic laser amygdalohippocampotomy (SLAH) is a minimally invasive surgical treatment for medically refractory medial temporal lobe epilepsy (MTLE) that has comparable rates of seizure freedom to traditional resective MTLE surgery. The psychiatric outcomes of epilepsy surgery need to be considered due to the high overall prevalence of psychopathology in epilepsy patients. Though psychiatric outcomes after resective epilepsy surgery have been frequently examined, the current study is the first to describe psychiatric outcomes after SLAH. The objective of this study was to (1) determine the changes in depression and anxiety in MTLE patients after SLAH; (2) identify patient characteristics associated with worsening depression or anxiety following SLAH; and (3) determine the prevalence of de novo psychopathology after SLAH. Methods: Medical records of 38 MTLE patients undergoing SLAH between 2011 and 2016 were retrospectively reviewed focusing on Beck Psychiatric Symptom Scales (Beck Depression Inventory-II [BDI-II] and Beck Anxiety Inventory [BAI]) preoperatively and 6 months following surgery. Two-tailed Wilcoxon signed-rank tests were used to determine whether there were significant changes in depression or anxiety symptoms after surgery. Beck scores were then dichotomized into worse symptoms (postoperative score - preoperative score > 0) or same/better symptoms (postoperative score - preoperative score = 0) following SLAH. Pre-surgical seizure characteristics, postoperative seizure outcome, psychiatric history, and medication use were identified. Univariate association analyses were conducted to identify variables associated with worse depression or anxiety symptoms following SLAH. The prevalence of de novo psychopathology following SLAH was determined by evaluating how many patients with no pre-surgical lifetime psychiatric history were taking psychotropic medications postoperatively. Results: Our study demonstrated an overall 4.5 point median decrease in BDI-II scores (p = 0.15) and 3.0 point median decrease in BAI scores (p = 0.03) following SLAH (Table 1), yet 14 patients (37%) experienced worse depression symptoms and 9 patients (24%) had worse anxiety symptoms. Younger age (p = 0.08) and a pre-surgical history of secondarily generalized tonic-clonic seizures (p = 0.06) were associated with worse depression after surgery. There was no relationship between laterality of surgery, seizure freedom, or lifetime psychiatric history and depression or anxiety outcomes. Two of 17 (12%) patients with no lifetime psychiatric history developed de novo psychopathology following SLAH. Conclusions: This study is the first to evaluate psychiatric outcomes after SLAH. SLAH may improve overall psychiatric symptoms, similar to traditional resective MTLE surgery, but de novo psychopathology and postoperative psychiatric morbidity remain significant issues. Further investigation is required to identify patients at risk for psychiatric morbidity following SLAH. Funding: Not applicable