Comparison of Neuropsychometric Results Before and After Resective Pediatric Epilepsy Surgery
Abstract number :
1.347
Submission category :
9. Surgery / 9B. Pediatrics
Year :
2018
Submission ID :
502644
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Kenney-Jung Daniel, Mayo Clinic; Kirsch Alexandra, Mayo Clinic; Michael Zaccariello, Mayo Clinic; Tanya Brown, Mayo Clinic; Benjamin H. Brinkmann; Eric T. Payne, Mayo Clinic; Katherine C. Nickels, Mayo Clinic; Elaine Wirrell, Mayo Clinic; and Lily Wong-Ki
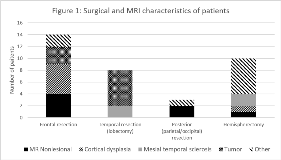
Rationale: While resective epilepsy surgery is the standard of care for selected patients with medically refractory focal epilepsy, concern exists for the neurodevelopmental consequences of brain resection in the pediatric age group. Methods: A retrospective cohort of pediatric patients who had undergone resective epilepsy surgery and who had had neuropsychological evaluation (NPE) before and after surgery was identified. Standard scores assessing global intellectual functioning, verbal and nonverbal intellectual ability as well as academic ability (spelling, word reading and mathematical ability) were abstracted from studies before and after surgery, and compared with respect to surgery lateralization and localization (temporal, extratemporal or hemispherectomy). The Behavior Assessment for Children (BASC) parental questionnaire was also examined, to assess the subject’s behavioral status from the caretaker’s point of view. Testing data were compared using the paired Student’s t-test, with unpaired data points being discarded for each analysis. Results: Thirty-four patients (61.8% male) who had undergone NPE before and after epilepsy surgery were identified. The median age at the time of surgery was 9.29 years (range 2-18.5 years). Imaging and surgical characteristics among this cohort may be seen in Figure 1.The median time between the first NPE and surgery was 54 days (IQR 19-120) and the median time elapsed between surgery and the second test was 257 days (IQR 182-372). The mean number of anti-seizure drugs (ASDs) used was 2.3 during the first NPE and 1.8 ASD at the second NPE.No statistically significant difference was found among the standard scores or BASC scores before and after epilepsy surgery (Table 1). The postsurgical and presurgical global intellectual scores (FSIQ) among the six patients who were not seizure-free at the second NPE were similar to patients whose seizures were controlled, with median presurgical FSIQ of 74 (IQR 51-92) and median postsurgical FSIQ of 78 (IQR 51-94) for the seizure-free group (n = 19) versus a presurgical median FSIQ of 73 (IQR 65.25-82.25) and postsurgical median FSIQ of 75.5 (IQR 60.5-89) for the non-controlled group (n = 6) . Significant group-level changes in global intellectual functioning before and after surgery were not seen with temporal or extratemporal resective surgery or with hemispherectomy (Table 1). Conclusions: As a group, children who underwent resective epilepsy surgery showed stable neuropsychometric results at short-to-medium term follow-up without deleterious consequences to development. Presurgical and postsurgical NPE for pediatric epilepsy surgery candidates should be routinely performed with continued long-term follow up to elucidate the developmental trajectories of these patients. Funding: None
.tmb-.png?Culture=en&sfvrsn=28cfc1d0_0)