Consensus Polling in Epilepsy Surgery Conference – Does It Improve the Surgical Discussion?
Abstract number :
3.347
Submission category :
9. Surgery / 9C. All Ages
Year :
2018
Submission ID :
497722
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Wynne Bird, Children's Hospital Colorado; Kevin E. Chapman, Children’s Hospital Colorado, University of Colorado School of Medicine; and Charuta Joshi, Children's Hospital Colorado
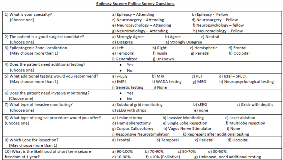
Rationale: Every patient that is in the epilepsy surgical pathway is presented at our interdisciplinary epilepsy surgery care conference (ESC) for surgical consensus. The final discussion regarding epilepsy surgery with families occurs after the patient has been presented at ESC. Epilepsy, neurosurgery, neuropsychology, and neuroradiology providers all give input into this discussion. All data related to the patient’s epilepsy management and clinical tests results are presented. Open group discussion occurs after presentation to develop a consensus as to what surgical option may be recommended to the patient. At times, this discussion can get sidetracked or confusing with multiple opinions being discussed so that a concise plan is not formed. Methods: A survey was developed to provide equal opportunity for individual provider recommendations and to document a concise plan for the patient. This survey included questions regarding: provider specialty, surgical candidacy, type of surgery recommended, additional testing recommendations, and predicted percentage of seizure freedom rate at 1 year regarding the surgical option the provider chose. The survey results are then open for discussion during the conference for further clarification of the consensus if it was not unanimous regarding surgical recommendations. The final survey data is then sent to the epilepsy presenter for documentation of the recommended surgical plan. After 6 months of utilizing the conference survey, a utility survey was sent to all providers. This survey included questions regarding: provider specialty, survey utility, if it changed provider discussion with the patient, if it improved and decreased discussion time at conference, and any suggestions for changing the survey. During the survey collection no identifying patient data was collected. Results: We had epilepsy, neurosurgery, and neuropsychology providers respond to the utility survey. 92% of the providers felt the surgical conference survey was very useful/useful. 90% felt the survey sometimes/frequently changed their management plan. 86% agreed/strongly agreed the survey has substantially reduced the time for the decision making process during conference. 78% gave feedback on improving the survey to improve conference discussion. Conclusions: Consensus polling survey during epilepsy surgery care conference streamlines medical discussion and recommendations for surgical interventions. We continue to apply our polling survey and are looking at implementing future polling options to improve communication and patient discussions. Funding: None
.tmb-.png?Culture=en&sfvrsn=bf1f50e0_0)