Critical care of pediatric refractory convulsive status epilepticus. Results from the Pediatric Status Epilepticus Research Group (pSERG)
Abstract number :
3.321
Submission category :
Late Breakers
Year :
2013
Submission ID :
1864688
Source :
www.aesnet.org
Presentation date :
12/7/2013 12:00:00 AM
Published date :
Dec 5, 2013, 06:00 AM
Authors :
H. Goodkin, N. Abend, S. Agadi, S. An, R. Arya, R. Basu, J. Brenton, J. Carpenter, K. Chapman, W. Gaillard, T. Glauser, M. Mikati, K. Peariso, M. Ream, G. Rathore, I. S nchez Fern ndez, R. Tasker, T. Loddenkemper
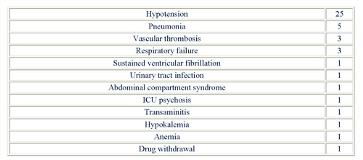
Rationale: The critical care of pediatric patients with refractory convulsive status epilepticus (RCSE) is based on limited data. The aim of this study was to describe the treatment strategies, complications, and outcomes in the critical care of pediatric patients with RCSE.Methods: The Pediatric Status Epilepticus Research Group (pSERG) is a multicenter network of reference hospitals that collects information from children with RCSE. Patients were included if: 1) Aged 1 month to 21 years, 2) convulsive seizures at onset, 3) failure of two or more antiepileptic drugs (AEDs) or the initiation of continuous administration of AEDs to abort seizures. Patients were excluded if: 1) non-convulsive SE (NCSE) detected on electroencephalogram (without convulsive seizures at onset), or 2) NCSE and infrequent myoclonic jerks.Results: 96 RCSE episodes were analyzed in 93 patients (48 males and 45 females). The median (p25-p75) age at the episode was 3.2 (1.2-8.2) years. At the time of presentation, 30 (31.3%) episodes were continuous (prolonged, single seizure) and 66 (68.8%) were intermittent. Seventy-three episodes (76%) required intubation. The median time of mechanical ventilation was 48 (14-144) hours. Forty-five episodes (46.9%) required neuromuscular blockade. Continuous intravenous medication infusions were given in 45 episodes (46.9%), with midazolam (35 episodes, 77.8%) being the preferred initial option. A second continuous infusion was required in ten episodes including pentobarbital in 5 (50%). Five of these 10 episodes necessitated a third continuous infusion and 1 a fourth. Hypotension occurred in 25 episodes (26%), requiring fluid boluses in 21 (84%) and vasoactive medications in 17 (68%). Four episodes (4.2%) were associated with cardiac arrest, which was reversible in three and lethal in one. All complications associated with RCSE are listed in Table 1. The median intensive care unit (ICU) length of stay was 3 (2-10) days. At the time of hospital discharge, patients returned to baseline function after 66 episodes (68.8%), did not after 26 episodes (27.1%), and the degree of functionality post-RCSE was unclear in 4 episodes (4.2%). Four RCSE episodes (4.2%) were lethal prior to discharge from the ICU. Conclusions: Three-fourths of pediatric patients with RCSE required intubation and almost half required continuous infusions of AEDs. Complications were common and severe, but approximately two-thirds of patients returned to baseline after RCSE and only a minority died.