Electrographic Status Epilepticus as a Presentation of a Patient With Hemiplegic Migraine
Abstract number :
3.184
Submission category :
4. Clinical Epilepsy / 4B. Clinical Diagnosis
Year :
2018
Submission ID :
502627
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Modhi Alkhaldi, Epilepsy Center, University Hospitals Cleveland Medical Center; Rita Martins, Doutor Fernando Fonseca; Faisal Almayman, University Hospitals Cleveland Medical Center; Guadalupe Fernandez-Baca Vaca, Epilepsy Center, University Hospitals Cle
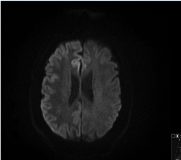
Rationale: A strong relationship between epilepsy and familial hemiplegic migraine(FHM)has been recently described in the literature. FMH is a rare clinically heterogenous monogenic subtype of migraine with aura, characterized by attacks of transient motor weakness and other various neurologic features. The mutations in geneATP1A2(FHM2) are associated with a high incidence of epilepsy and severe attacks. Methods: We report a case of FHM2 presented with focal nonconvulsive status and severe encephalopathy 54-year-old right-handed Caucasian male with intellectual disability and history of complex migraine presented with electrographic status epilepticus(SE) did not improve with antiepileptic drugs (AEDs). He also had persistent left-sided hemiplegia for days as he presented with a headache, confusion and alternating weakness. His initial EEG and MRI brain were normal. On exam, he is disoriented, has left facial droop, visual and motor neglect on the left side. Repeat MRI brain was positive for diffusion restriction of the right hemisphere with cortical edema and gadolinium enhancement. MRA showed increased vascularization of the right hemisphere. EEG showed electrographic focal SE from the right tempro-parital area. Further history revealed that he had several similar episodes since the age of 2 with invariably negative neurologic workup including stroke and mitochondrial disease. Family history is negative for hemiplegic migraine but many members have epilepsy and/or migraine. He was started on methylprednisolone with remarkable improvement. Genetic testing for hemiplegic migraine was positive for ATP1A2 exon16, C2143G>A(p.GLY715 Arg) heterogeneous missense mutation. On follow up visits, he returned to his baseline. Results: Epilepsy has been reported in all three FMH types with a higher frequency in ATP1A2andSCNA1gene mutations, reflecting a genetically determined dysfunction of neuronal ion transporters. In these phenotypes, seizures may occur independently of hemiplegic migraine attacks. However, the mechanism of status epilepticus triggered by disease flairs is unclear and may be related with transient cerebral edema and cortical spreading depression that result in synchronous neuronal hyperexcitability. Genetically determined dysfunction of sodium-potassium ATPase pump resulting in hyperexcitability with increased glutamate in the synaptic space. Our patient presented with focal electrographic status with marked right hemispheric cytotoxic edema and diffusion restriction that leads to a broad differential diagnosis, including stroke and autoimmune encephalitis. However, his past medical history of seizures in neonatal period and childhood and migraine with aura led to considering the diagnosis of FHM. Given the severity of the hemiplegic attack and absence of therapeutic efficacy of AEDs, high-dose corticosteroid was started. A marked improvement observed at the second day of treatment. Conclusions: Our case emphasizes the importance of obtaining detailed history in leading to the correct diagnosis in a patient presenting with a first episode of status epilepticus. It also suggests testing patients with prolonged hemiplegic migrainous attacks and confusion with continuous EEG to ascertain whether electrographic status is occurring. To our knowledge, this is the first case report of FHM with an improvement of both clinical, neuroimaging and SE with corticosteroids in the absence of response to AEDs.L.Deprez et al.Epilepsy as part of the phenotype associated with ATP1A2 mutations, Epilepsia, 49(3):500–508, 2008 Zangaladze et al.Epilepsy & Behavior 17 (2010) 293–295, Sporadic hemiplegic migraine and epilepsy associated with CACNA1A gene mutation. Funding: Not applicable
.tmb-.png?Culture=en&sfvrsn=8ae38724_0)