In Search of Biomarkers for the Epileptogenic Zone: A Machine Learning Approach
Abstract number :
3.035
Submission category :
1. Basic Mechanisms / 1C. Electrophysiology/High frequency oscillations
Year :
2018
Submission ID :
502570
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Olesya Grinenko, Cleveland Clinic; Jian Li, University of Southern California; John C. Mosher, Cleveland Clinic; Juan Bulacio, Cleveland Clinic; Jorge A. Gonzalez-Martinez, Epilepsy Center, Neurological Institute, Cleveland Clinic; Imad M. Najm, Cleveland
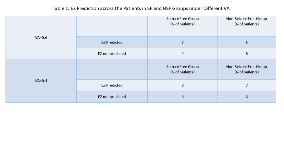
Rationale: A specific time-frequency pattern of the epileptogenic zone (EZ) has been identified [1]. This pattern encompasses the inter-ictal to ictal transition and consists of three main components: initial sharp transient(s) or spike(s) then fast activity and simultaneous low-frequency suppression. We developed a support vector machine (SVM)-based approach to automatically detect the pattern and differentiate EZ from the regions of propagation. Originally the machine learning system was trained and cross-validated on a group of 17 patients that were seizure free (SF) after surgery. We were able to identify EZ in 15 out of 17 patients and achieve 90.6% positive predictive value (PPV) and 0.7% false positive rate (FPR) (Table 2 in [1]). The current study aims at extending and validating the algorithm on a completely independent series of patients that were drawn consecutively from 2015. The results between the SF and NSF (non-seizure free) groups of patients were analyzed for comparison. Methods: 24 consecutive patients who underwent SEEG evaluation at the Cleveland Clinic and had seizure onset characterized by beta or gamma activity were included in this study. All patients underwent surgical resection, 11 became SF and 13 remained NSF. We applied the previously trained SVM-based model [1] to both groups of patients and analyzed all available seizures that met the inclusion criteria. Results: Our algorithm identified EZ in 7 out of 11 SF patients and in 5 out of 13 NSF patients (see Table 1 for details). In the SF group, EZ was identified only inside the resection in 5 patients, inside and outside the resection in 2 patients. In total 29 out of 33 electrode contacts identified as EZ were localized inside the resection area, resulting in 87.9% PPV and 0.47% FPR. In the NSF group, EZ was identified only outside the resection in 3 patients, inside and outside the resection in 2 patients. In total 21 out of 81 electrode contacts identified as located in EZ were localized inside the resection (see Table 2 for details).One patient (subject 219) from NSF group underwent a second surgery and became seizure-free after complete resection of the EZ that was detected by the classifier.The time-frequency ictal pattern could vary across multiple seizures for a single subject. Also, the previously trained model was very conservative. Hence, in order to improve EZ detection, we lowered the voting agreement (VA) from the original 0.6 to 0.4 that resulted in identifying more EZ electrode contacts inside the resection for SF group and outside the resection for NSF group, without sacrificing the detection power. Conclusions: The previously developed machine learning algorithm was validated on an independent series of patients. The results for the NSF group showed that including the predicted EZ into the resection can be critical for seizure freedom. Detected EZ was more localized in SF rather than NSF patients. This may be due to an inappropriate placement of the implanted SEEG electrodes or due to a different type of EZ organization (unstable and more extended) in this group.Reference[1] Grinenko O, et al. A fingerprint of the epileptogenic zone in human epilepsies. Brain. 2018;141(1):117-131.*Olesya Grinenko and Jian Li contributed equally to this work. Funding: National Institutes of Health under award R01NS089212 and R01EB009048
.tmb-.png?Culture=en&sfvrsn=308a8a60_0)