Incidence of Hypertension in Children Treated With ACTH or Prednisolone for Infantile Spasms
Abstract number :
1.314
Submission category :
7. Antiepileptic Drugs / 7D. Drug Side Effects
Year :
2018
Submission ID :
499858
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Laurel McGarry, Children's Hospital Colorado; Ricka Messer, Children's Hospital Colorado; and Kelly Knupp, University of Colorado Children's Hospital Colorado
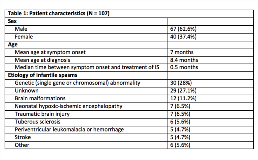
Rationale: Children with infantile spasms (IS) are often treated with adrenocorticotropic hormone (ACTH), which has numerous systemic side effects including hypertension (HTN) and, rarely, fatal cardiomyopathy. Our institution recommends close monitoring for HTN with initiation of antihypertensive treatment and echocardiogram (echo) for children on ACTH or prednisolone who develop HTN; however, the incidence and sequelae of HTN in this population are poorly understood. Methods: A retrospective chart review was performed at a single institution. Children aged 2 months-3 years with newly diagnosed IS treated from January 2013-October 2017 were included. Patients who received treatment at another center or had a pre-existing diagnosis of HTN, significant cardiac disease, or renal disease were excluded. Variables collected included age, sex, etiology of IS, treatment of IS, documented diagnosis of HTN in the medical record, missed diagnosis of HTN, treatment of HTN, echo performed, echo abnormalities, referrals made for HTN, and whether HTN was persistent 2 months after treatment. Missed diagnosis was defined as 3 recordings of blood pressure greater than 95th% for age, sex, and height over three checks without a documented diagnosis. Analyses included descriptive statistics with %, means, and medians. Differences between groups were assessed using chi-square. Results: Of the 107 patients included, 77 were treated with ACTH (maximum dose of 125-150 units/m2/day for two weeks), 11 with prednisolone (maximum dose 4-8 mg/kg/day for two weeks), and 22 with non-steroidal therapy (vigabatrin or topiramate). HTN occurred in 34 children (44%) treated with ACTH (27 with a documented HTN diagnosis and 7 missed diagnoses) and 3 (37.5%) of those treated with prednisolone (2 documented and 1 missed diagnosis). No child treated with non-steroidal therapy developed HTN. The incidence of HTN between ACTH and prednisolone groups was not significantly different (p=0.63). In contrast, the incidence of HTN was significantly higher in the ACTH group compared to the non-steroidal group (p=0.0001) and in the prednisolone group compared to the non-steroidal group (p=0.003). Antihypertensive treatment was started for 25 children (86%) diagnosed with HTN, and 6 required multiple antihypertensive medications. Early reduction in dose or discontinuation of ACTH/prednisolone occurred in 7 children, including 1 child without a documented diagnosis of HTN. No changes were made for the other 7 patients with missed HTN diagnoses. Echo was performed in 15 children, with no cases of cardiomyopathy and 5 minor abnormalities. Three children were admitted to the hospital for HTN. Two children had persistent hypertension at two months after discontinuation of ACTH. Conclusions: HTN is a common side effect of steroidal therapy for IS, occurring in nearly half of children treated with ACTH and over one third of those treated with prednisolone. Persistent HTN following discontinuation of ACTH was rare, and none of the children developed cardiomyopathy, regardless of whether HTN was treated. Further study is needed to determine the role of anti-hypertensive treatment for ACTH-related HTN. Funding: No funding was received in support of this abstract.