Insular Plus Epilepsy and Surgical Treatment
Abstract number :
1.345
Submission category :
9. Surgery / 9A. Adult
Year :
2018
Submission ID :
507393
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Niravkumar Barot, Thomas Jefferson University; Maromi Nei, Thomas Jefferson University; Scott Mintzer, Thomas Jefferson University; Christopher Skidmore, Jefferson Comprehensive Epilepsy Center, Thomas Jefferson University; and Michael Sperling, Jefferson
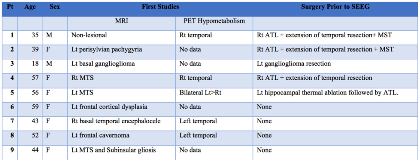
Rationale: Epileptogenic insular cortex is challenging to diagnose and treat because of its deep location, dense connections, and overlying vascular structures. With the use of stereotactic electroencephalography (SEEG), a detailed investigation of insular involvement in cases with or without known MRI reported lesions can be achieved. Here, we report the patient characteristics and outcome in cases of SEEG-documented ictal onset involving the insula with or without MRI reported lesions who had surgical resection of insular cortex. Methods: Insular implantation was done in 27 cases from December 2014 to June 2017, with 10 patients demonstrating initial ictal discharges in insular contacts. Nine patients had the insular resection. Surgical resection could not be performed in one patient due to anatomic limitation. The outcome was defined based on modified Engel classification. We studied the phase I investigation, SEEG, surgical resection data and outcome at the last visit. Results: The mean age of nine study patients was 44.7 years [Range: 18-59 years] and seven were female. MRI showed mesial temporal sclerosis(MTS) in 2 patients and was unremarkable in one patient. The other 6 patients had different lesions (basal temporal ganglioglioma, frontal cavernoma, frontal cortical dysplasia, perisylvian polymicrogyria, basal temporal encephalocele and the dual pathology of MTS plus subinsular gliosis) Out of 9 patients who underwent SEEG evaluation, 5 of them had had prior resective surgery in the temporal lobe based on reasonably concordant phase I investigations but failed to achieve seizure freedom. SEEG evaluation after failed resection in 3 of these patients revealed seizures starting in insular contacts, while two patients had seizures beginning independently in the insula and in the temporal lobe.The remaining 4 patients had had no prior surgeries. Two had frontal MRI lesions outside the insula, but SEEG showed seizures starting either in insula with very rapid spread to the lesion or synchronous onset in the insula and lesion; surgical resection involved insular cortex and lesions in both patients. The third patient showed seizures starting in the hippocampus and insular cortex, contralateral to the encephalocele, which was therefore considered an incidental finding. She underwent anterior temporal lobectomy plus resection of the involved insular cortex. The fourth patient with dual pathology of subinsular gliosis and left MTS had ictal onset in the insular contacts. She underwent insular resection and left anterior temporal lobectomy.After insular cortex resection, 6 of the 9 patients achieved class I outcome at the last follow up visit with a mean follow up duration of 21 months (4-38 months, 4/7 patients with > 12 months follow-up were class 1). Two patients had class 3 outcome, and 1 had class 4 outcome. The only finding suggestive of outcome was the presence of contralateral interictal spikes on scalp EEG, which was seen in two out of three patients with poor outcome and absent among patients with class 1 outcome. Conclusions: The insula may be a critical part of the epileptogenic network in patients with extra-insular MRI lesions. SEEG evaluation of the insula should be considered in patients who fail lesion resection and is worthwhile in some patients with lobar lesions if malformation of cortical development or more multilobar injury is present. More research is needed to determine which patients are optimal for insular investigation. Funding: Not applicable
.tmb-.png?Culture=en&sfvrsn=66684b60_0)