Interictal Epileptiform Activity During Rapid Eye Movement Sleep in the Epilepsy Monitoring Unit as a Predictor of Patient Outcomes
Abstract number :
1.239
Submission category :
4. Clinical Epilepsy / 4D. Prognosis
Year :
2018
Submission ID :
479348
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Marna B. McKenzie, University of Manitoba and Marcus C. Ng, University of Manitoba
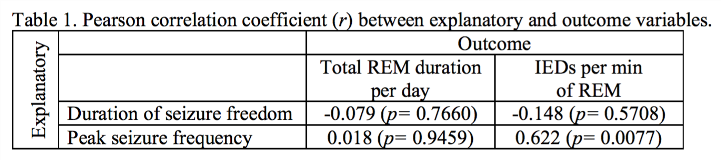
Rationale: The natural history of epilepsy is highly variable and aside from a few well-characterized epilepsy syndromes, accurate predication of disease course remains challenging. Different sleep states have been shown to influence both seizure onset and interictal epileptiform activity. Given that REM sleep is generally inhibitory to seizures and interictal epileptiform discharges (IEDs), we hypothesize that patients with breakthrough seizures and IEDs during REM sleep will have more refractory and aggressive epilepsy, suggesting an overall poorer prognosis. Methods: EEG recordings from 63 patients in the adult Epilepsy Monitoring Unit (EMU) over a 12-month period were retrospectively analyzed to determine the frequency of IEDs during REM sleep and the total amount of REM sleep recorded in each individual over the duration of their stay in the EMU. Frequency of IEDs was measured as the mean duration of IEDs (in 1-second intervals) per minute of REM sleep. A detailed-chart review of all 63 patients was performed in the four year period surrounding EMU admission (date of admission +/- 2 years). Data collected included: peak seizure frequency, longest duration of seizure freedom, seizure types and occurrence of status epilepticus. Results: There were 63 patients diagnosed with epilepsy included in the study. The preliminary analysis of the first 17 patients suggests there is a significant, moderate-strong positive relationship between the duration of IEDs per minute of REM sleep, and a patient’s peak seizure frequency (Pearson r=0.622, p=0.0077), results in table 1. Conclusions: The preliminary results of the first 17 patients in the study suggest there is a positive linear relationship between duration of IEDs in REM sleep in the EMU, and a patient’s peak seizure frequency in the 2 years preceding and after an EMU admission. With the final analysis of all 63 patients, we will have higher power to better assess additional relationships between (1) the frequency of IEDs during REM sleep and other outcome variables (longest duration of seizure freedom, seizure types and occurrence of status epilepticus), and (2) the duration of REM sleep and all outcome variables (peak seizure frequency, longest duration of seizure freedom, seizure types and occurrence of status epilepticus). Determining the predictive power of both the frequency of IEDs during REM sleep and duration of REM sleep holds great prognostic value and would be extremely helpful in clinical management and patient education. Funding: This work was supported by the University of Manitoba Bachelor of Science in Medicine program.