Mid-Level Providers’ Contribution to Epilepsy Monitoring Unit
Abstract number :
3.425
Submission category :
13. Health Services (Delivery of Care, Access to Care, Health Care Models)
Year :
2018
Submission ID :
502271
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Hae Won Shin, University of North Carolina; Shabina Sheikh, UNC Health Care; Disha Miyani, UNC Healthcare; Linh Ngo, UNC Health Care; Joyce Kern, UNC Healthcare; Heather Ritchie, UNC Healthcare; Jane Kwon, University of North Carolina; Albert Hinn, Univer
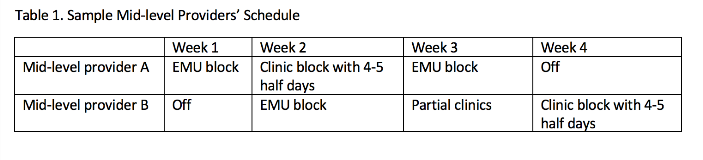
Rationale: More hospitals and health care systems are utilizing mid-level providers to reduce the costs but improve the efficiency. Epilepsy centers are not exception for this new health care environment. Yet, there is no systematic study to show the addition of mid-level providers to add values in epilepsy monitoring unit (EMU). As a NAEC level 4 academic epilepsy center, University of North Carolina (UNC) recently added two mid-level providers to EMU with infrastructure change. We aim to show the values of such change. Methods: In May 2017, UNC EMU changed the structure with addition of 2 mid-level providers. Previously EMU was covered by general ward team, consisting of vascular neurologist as an attending physician, neurology and psychiatry resident physicians and epileptologist as a consultant. New EMU model was covered by an epilepsy team, consisting of epileptologist as an attending physician, epilepsy fellow physician and a mid-level provider. Two mid-level providers were added so that one provider is in EMU 7 days per week while the other provider is either having partial clinic days or having days off. Total costs of addition of two mid-level providers are compared to total expected professional revenue to the epilepsy program. Total admissions to EMU from May 2017 till April 2018 are compared to the total admissions from May 2016 till April 2017. Random 50 patients’ discharge time in each time period is compared to show efficiency. Results: Total compensation costs to add 2 mid-level providers are $242,233. Projected revenue growth compared to previous year by adding mid-level providers are $ 253,096, including increased clinic access and throughput to EMU with increased vEEG (CPT code of 95951) charges and inpatient E&M charges. For outpatient clinic growth contribution, we are able to provide additional up to 10 half day epilepsy clinics per month by adding mid-level providers as seen in Table 1 of mid-level providers’ schedule. Total EMU admissions from 5/2016 to 4/2017 are 153 while the total EMU admissions from 5/2017-4/2018 are 228 with 49% increased volume, which is more than expected. Addition of mid-level provider with EMU infrastructure contributed earlier discharge time by 50 minutes on average which saves total 8 hospital days. Conclusions: Non-academic and academic epilepsy centers have utilized the mid-level providers for their inpatient and outpatient care. Recent UNC epilepsy center change with 2 additional APPs have shown the financial feasibility to grow the outpatient and inpatient program by adding resources and improvement of efficiency by earlier discharge time. Funding: None
.tmb-.png?Culture=en&sfvrsn=8fc985b8_0)