Pathology Underlying Drug-Resistant Epilepsy in the Elderly and the Influence of Age of Epilepsy Onset
Abstract number :
2.403
Submission category :
14. Neuropathology of Epilepsy
Year :
2018
Submission ID :
501291
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Angela Crudele, Cleveland Clinic Foundation; James Bena, Cleveland Clinic Foundation; Andrey Stojic, Cleveland Clinic Foundation; Richard Prayson, Cleveland Clinic Foundation; and Vineet Punia, Cleveland Clinic Foundation
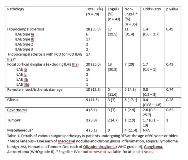
Rationale: A rapidly aging population in combination with elevated risk of epilepsy in the elderly is likely to increase the number of elderly patients with drug resistant epilepsy (DRE) who are potential resective epilepsy surgery (RES) candidates. We recently reported seizure outcomes after RES among patients older than 60 years to be comparable to younger adults (25 – 45 years old). However, not much is known about the pathology underlying DRE in elderly population undergoing RES. This is the aim of our study along with investigating the influence of age of epilepsy onset on the type of pathology. Methods: After IRB approval, we searched our prospectively maintained database to identify patients who underwent RES for DRE at the age of =60 years between 1/1/2000 and 03/30/2018. Available microscopic slides were reviewed by a dedicated neuropathologist in all cases. ILAE criteria for classification of hippocampal sclerosis (HS) and focal cortical dysplasia (FCD) were used. Due to clinical relevance, MRI positive HS was classified as such on pathology, despite an associated FCD (not classified as FCD ILAE IIIa). Appropriate descriptive statistical methods were used to analyze the data. The interaction of age of epilepsy onset with pathology was analyzed using receiver operating characteristic (ROC) curve analysis. Results: A total of 78 patients (59% females) were included. The mean age at the time of RES was 64.7 (±3.7) years and of epilepsy onset was 37.4 (±20.8) years. Temporal lobectomy was the most common (71.8% patients) RES. The most common pathologies included HS (35.9%), FCD (25.6%) and remote infarct/ischemic changes (12.8%) (Table 1). There were 18 (23%) patients with dual pathologies and 1 patient with triple pathology (HS, FCD and a remote infarct). ROC analysis showed that only HS had a significant correlation with epilepsy onset age with an odds ratio of 0.96 (p = 0.002). The best cutoff for predicting HS pathology was 43 years (shown in Figure 1) with a sensitivity and specificity of 0.75 and 0.62, respectively. While 52.5% of patients with epilepsy onset prior to the age of 43 were found to have HS, only 18.4% with a later onset had this pathology. Among 14 patients with epilepsy onset at the age of =60 years, none had HS. There were 55 (70.5%) patient with at least 1 year clinical follow-up and 43 (78.2%) of them achieved Engel I outcome at the last follow-up. There was no difference in pathology between patients with Engel I outcome and the rest (follow-up <1 year or Engel II – IV outcomes; Table 1). Conclusions: The most common pathology among patients undergoing RES at the age of =60 years, consistent with historically reported younger adults, was HS. However, its presence seems to be influenced by the age of epilepsy onset. For each year increase in age of epilepsy onset, the odds of HS as an underlying pathology decreased by 4%. Patients with age of onset of later than 43 years were significantly less likely to have HS compared to their younger counterparts. Funding: Not applicable.
.tmb-.jpg?Culture=en&sfvrsn=c0688689_0)