Predicting Postoperative Language Outcome Using DWI, fMRI, and MEG
Abstract number :
3.256
Submission category :
5. Neuro Imaging / 5B. Functional Imaging
Year :
2018
Submission ID :
505786
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Abbas Babajani, University of Tennessee Health Science Center; Christen M. Holder, The University of Tennessee Health Science Center; Adeel Siddiqui, University of Tennessee Health Science Center; and Asim Choudhri, University of Tennessee Health Science
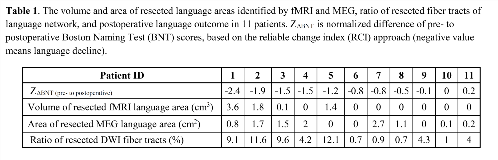
Rationale: Presurgical language mapping is usually performed to minimize the risk of postoperative impairment after epilepsy and tumor surgery. In our recent study, we found that a larger extent of resected language area identified by functional MRI (fMRI) and magnetoencephalography (MEG) was associated with more postoperative language deficit [1]. Diffusion-weighted imaging (DWI) can identify pathways originating from Broca’s and Wernicke’s areas, and damage to these pathways can lead to deficits in multiple language functions after epilepsy surgery. However, no study has yet investigated the predictive power of presurgical DWI for prediction of language outcome. The aim of this study was to compare the predictive power of DWI, fMRI, and MEG (in unimodal and multimodal approaches) for prediction of the postoperative language outcome. Methods: Of consecutive series of 26 patients who underwent epilepsy surgery, 11 patients (7 males; aged 24 ± 9 years) met inclusion criteria [1]. All patients received pre- and six-month postoperative neuropsychological evaluation of language using the Boston Naming Test (BNT) (Table 1). Presurgical language mapping using fMRI and MEG were described elsewhere [1]. We utilized fMRI activation as input regions of interest (ROIs) for identifying fiber tracts of the language network. The resected areas in all patients were identified. The volume of resected fMRI and MEG activations within the canonical language regions and the ratio of the number of resected language fibers to the total number of language fibers were used as input feature of a support vector regression (SVR) to predict the language outcome. The decline from pre- to postoperative BNT was the output of the SVR. SVR models were trained and cross-validated. We compared the cross-validation (CV) errors of the unimodal and multimodal SVR models to evaluate the predictive power of different modalities. Results: Results of neuropsychological evaluation revealed that 9 patients had some degree of postoperative language deficit (Table 1). Table 1 shows that patients with more language deficit had an overall more resected language areas identified by fMRI and MEG, and a larger ratio of resected fiber tracts of language network. The prediction errors of postoperative language outcome corresponding to different modalities are compared in Fig. 1. The error of DWI-SVR model was less than MEG-SVR model but larger than fMRI-SVR, although there was no significant difference between these errors (P > 0.09). The error of a multimodal SVR model comprising DWI, fMRI, and MEG was smaller than the unimodal SVR models and this error was significantly smaller than the error of DWI- and MEG-SVR models (P < 0.05). Conclusions: Considering limitations of invasive presurgical language mapping methods, it is highly desirable to have additional presurgical language mapping method based on noninvasive modalities. Our results revealed a multimodal presurgical language mapping approach based on DWI, fMRI, and MEG can provide an accurate and reliable prediction for postoperative language outcome.Reference[1] Babajani-Feremi A. et al. Clinical Neurophysiology, 2018;129:560-571. Funding: The Children’s Foundation Research Institute & The Shainberg Neuroscience Fund, Memphis, TN
.tmb-.png?Culture=en&sfvrsn=683c1a9_0)