Psychogenic Non-Epileptic Seizures (PNES) – Inpatient Trends and Psychiatric Comorbidities
Abstract number :
3.428
Submission category :
16. Epidemiology
Year :
2018
Submission ID :
501299
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Urvish Patel, Creighton University School of Medicine; RamMohan Sankaraneni, Creighton University School of Medicine; and Sanjay Singh, Creighton University School of Medicine
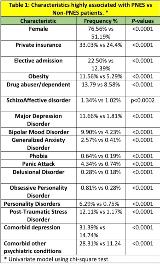
Rationale: Psychogenic non-epileptic seizures (PNES) represent a significant neuropsychiatric condition. The incidence of PNES is estimated to be between 1.4-4.9/100,000/year and the prevalence is between 2 to 33 per 100,000. There is very limited data on the profile of these PNES patients that are hospitalized, even though it is their hospitalization that is responsible for a significant part of their cost of their care. These hospitalized PNES patients also present a unique opportunity to study their psychiatric comorbidities in a more scientific manner. Here we looked at a sample of over 2 million epilepsy admissions. Methods: We performed a retrospective analysis of the Nationwide Inpatient Sample (years 2003-2014) in adult hospitalizations for Epilepsy using ICD-9-CM codes. We extracted patients with PNES and Non-PNES to compare the cost, LOS, and concurrent psychiatric conditions. A weighted univariate analysis was performed using chi-square, student t-test, and Cochran Armitage trend test. A multivariable survey logistic regression model, weighted to account for sampling strategy, with the predictors of PNES in epilepsy hospitalizations was fitted, adjusting for the following: Demographic, patient and hospital level characteristics, CCI (Charlson Comorbidity Index), other comorbidities, concurrent psychiatric conditions like Schizophrenia (S), Schizoaffective disorder (SA), Major Depressive Disorder (MDD), Bipolar Mood Disorder (BMD), Generalized Anxiety Disorder (GAD), Phobia, Panic Attack (PA), Delusional Disorder (DD), Obsessive Personality Disorder (OCP), Personality Disorders (PD), and Post-Traumatic Stress Disorder (PTSD). Results: Amongst 2,156,577 epilepsy hospitalizations, 13,697 (0.64%) had PNES with an increase in trend (0.4% in 2003 to 0.77% in 2014; PTrend <0.0001). The V-EEG monitoring utilization was higher among PNES compared to non-PNES (21.51% vs 7.94; PTrend V-EEG <0.0001). There was no noticeable difference in median LOS (3 days vs 3 days) or cost ($17,133 vs $16,359). On univariate analysis, patients with PNES were significantly younger (mean age: 39-years vs 52-years) and there were more females than males with this diagnosis. PNES patients had a higher prevalence of obesity, drug abuser/dependent, SA, MDD, BMD, GAD, Phobia, PA, DD, OCD, PD, PTSD, comorbid depression, and comorbid other psychiatric conditions as compared to those epilepsy patients without PNES (Table 1). On regression analysis MDD, GAD, PA, PD, PTSD, private insurance, self-pay, obesity, comorbid depression, and comorbid other psychiatric conditions had higher odds of having PNES in compare to Non-PNES epilepsy patients (Table 2). Conclusions: PNES admissions represent a small number of total epilepsy admissions – 0.64% (13,697 out of 2,156,577). There is a trend of more admissions for PNES. The data confirms that V-EEG is the method of choice for PNES diagnosis. There is a significantly higher incidence of psychiatric co-morbidity in hospitalized PNES patients, particularly PTSD and major depressive disorder. This study represents the first large nationwide study of PNES patients. Funding: None
.tmb-.jpg?Culture=en&sfvrsn=4c2e9a64_0)