Research Education Needs for Pediatric Epilepsy Junior Faculty
Abstract number :
2.109
Submission category :
4. Clinical Epilepsy / 4A. Classification and Syndromes
Year :
2018
Submission ID :
502510
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Natasha Basma, Weill Cornell Medicine; Joseph Sullivan, University of California, San Francisco Benioff Children’s Hospital; Renee Shellhaas, C.S. Mott Children's Hospital, Michigan Medicine; Dennis Dlugos, Children’s Hospital of Philadelphia;
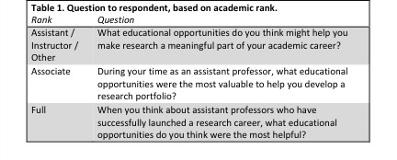
Rationale: There are many unanswered clinical questions in pediatric epilepsy across multiple domains, such as care quality, comparative effectiveness, epidemiology, genetics, and delivery of health services. In recent years, several consortia of pediatric epilepsy researchers have built active networks to gather data to answer these questions. To best make use of these new opportunities for research, there needs to be a workforce of pediatric epilepsy physicians with strong research skills. However, it is not clear what specific activities might be helpful for these individuals. Here, we sought to understand the research educational needs of junior faculty pediatric epilepsy physicians. Methods: We conducted (a) a focus group via teleconference and (b) an anonymous online survey to identify research educational gaps for junior faculty pediatric epilepsy physicians in academic centers. The survey was brief, and included specific questions for faculty at different levels of seniority in their academic careers (Table 1). We fielded the survey using SurveyMonkey.com. We applied thematic analysis to hand written notes taken during the teleconference, and to written responses to the survey. Results: The teleconference focus group included 20 individuals, all academic pediatric epilepsy specialists in US academic centers. There were 38 responses to the online survey, with representation of people at multiple levels of academic rank, including 16 (42%) instructor or assistant professors, 13 (34%) associate professors, 6 (16%) full professors, and 3 (8%) other. There were four major themes of reported educational needs, each with at least six responses. These were (1) formal coursework, especially in epidemiology and biostatistics; (2) opportunities for collaborative research; (3) mentorship; and (4) support for writing grants and manuscripts. In addition, five minor themes emerged, often with one or two responses. These were (1) protected time; (2) support from leadership; (3) grit (i.e. resilience in the face of adversity); (4) IRB support; and (5) financial guidance. (Table 2) Conclusions: There is good consensus among academic pediatric epilepsy physicians that junior faculty may benefit from a mix of formal educational opportunities (coursework in epidemiology, biostatistics, and clinical trials; help in writing grants and manuscripts) as well as from informal training through mentoring and collaborative research. In addition, protected time, leadership support, financial guidance, and IRB support may provide additional benefit. Effective mentorship and modeling of resilience in the face of failure (grit) are also a key support for junior faculty. Funding: None
.tmb-.jpg?Culture=en&sfvrsn=efb068e9_0)