Resection of Mesiotemporal Structural Anomalies and Its Relation to Surgical Outcome in Temporal Lobe Epilepsy
Abstract number :
2.182
Submission category :
5. Neuro Imaging / 5A. Structural Imaging
Year :
2018
Submission ID :
502419
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Fatemeh Fadaie, Neuroimaging of Epilepsy Laboratory, Montreal Neurological Institute and Hospital; Benoit Caldairou, Neuroimaging of Epilepsy Laboratory, Montreal Neurological Institute and Hospital; Seok-Jun Hong, Neuroimaging of Epilepsy Laboratory, Mon
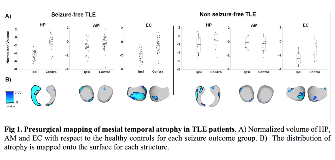
Rationale: Temporal lobe epilepsy (TLE) is the most common drug-resistant epilepsy in adults. Mesiotemporal lobe sclerosis (MTS), its histopathological hallmark, is reflected on MRI as hippocampal (HP), amygdalar (AM), and entorhinal cortex (EC) atrophy. While hippocampal atrophy on preoperative MRI is indicative of favorable outcome after surgery, long-term follow-up studies indicate that in up to 50% of patients seizures may recur (de Tisi et al.,2011,Lancet). Insufficient resection of the mesiotemporal lobe structures has been suggested as a key factor for unfavorable seizure outcome (Bonilha et al.,2007,Epilepsia). Yet, the relationship between extent of resected anomalies and outcome has not been evaluated. Here, we mapped the spatial overlap between preoperative MRI markers of MTS and their extent of resection on postoperative MRI to establish the criticality of feature combinations for outcome prediction. Methods: We obtained pre- and post-operative 3D T1-weighted MRI in 35 TLE patients (14 male, age=36 ±11) who underwent selective amygdalo-hippocampectomy (SAH) and 40 age and sex-matched healthy subjects. Patients were grouped into seizure free (SF; Engel I; n=26) and not seizure-free (NSF; Engel II-IV, n=9). We manually segmented the HP, AM and EC on the preoperative MRI. In addition to global volumetry, we generated surface-based representations and computed vertex-wise columnar volume (Kim et al.2008,MICCAI). Measures in patients were z-scored relative to controls and sorted into ipsi- and contralateral to the seizure focus. We carried out vertex-wise Student t-tests to map alterations in columnar volume in TLE-SF and TLE-NSF relative to controls. After registering the post- to the preoperative MRI, we calculated the proportion of tissue resected with respect to the total volumetric anomaly for each MTL structure (defined as z-score beyond 1.5 SD). These data were used by linear discriminant analysis (LDA), a supervised classifier, to predict post-surgical seizure outcome using 5-fold cross validation with 50 iterations. We repeated the analyses on an independent dataset of 20 TLE patients who underwent anterior temporal lobectomy (ATL), with 10 patients becoming SF and 10 NSF. Results: Compared to the healthy controls, both TLE-SF and TLE-NSF had ipsilateral mesial temporal volume loss (p0.01), although the distribution of HP atrophy was more widespread in TLE-SF (Fig 1). Moreover, a greater volume of abnormal HP and EC was resected in TLE-SF as compared to TLE-NSF (p0.01; Fig 2). LDA correctly predicted post-surgical seizure outcome in 73% of the patients when using a combination of resected volumes; among them, HP showed the highest predictive power (63%) followed by EC (55%), while prediction based on AM alone was at a chance level (48%). Findings from the ATL cohort were consistent with SAH both with respect to the pre-operative atrophy and its predictive value. Conclusions: Irrespective of the surgical approach, the main predictor for seizure freedom after ATL and SAH is the amount of excised morphologically abnormal hippocampal and entorhinal tissue. A precise delineation of MTL atrophy through advanced morphometry may also assist MRI-guided laser interstitial thermal therapy. Funding: MOP 57840 and 123520
.tmb-.png?Culture=en&sfvrsn=695d9f4e_0)