Seizure Induction by Direct Cortical Stimulation Predicts Postsurgical Outcome: A Two-Center S-EEG Study Combined With 3D MRI Analysis
Abstract number :
3.149
Submission category :
3. Neurophysiology / 3E. Brain Stimulation
Year :
2018
Submission ID :
505312
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Birgit Frauscher, Montreal Neurological Institute and Hospital; Nicolás von Ellenrieder, Montreal Neurological Institute and Hospital; Philippe Kahane, Grenoble-Alpes University Hospital; Ana-Sofia Hincapie, Montreal Neurological Institute and Hospit
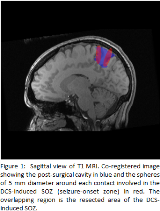
Rationale: Direct cortical stimulation (DCS) is widely used during intracerebral EEG work-up for patients with drug-resistant focal epilepsy. The rationale is that it helps in defining the cortical area responsible for seizure generation. No study, however, demonstrates that DCS contributes to a good surgical outcome. We investigated if removal of the DCS-induced seizure-onset zone (SOZ) as a marker for the epileptogenic zone is associated with a good postsurgical outcome. Methods: We studied consecutive patients who underwent stereo-encephalography (S-EEG) for presurgical evaluation at two tertiary epilepsy centers between 2007 and 2017. We selected patients who underwent DCS during implantation, who subsequently had open surgery with at least one year of follow-up and whose pre-implantation, implantation, and postsurgical brain imaging was available for analysis. We assessed the presence of ‘habitual’ electroclinical seizures (seizures resembling the patient’s spontaneous seizures as recognized by the patient/family or caregiver) induced by DCS. We defined the contacts involved in the DCS-induced SOZ and the spontaneous SOZ. We performed co-registration of the imaging studies. We created spheres of 5 mm diameter around each contact involved in both SOZs and marked the postsurgical cavity and calculated its volume (Fig. 1). The percentage of resected volume of the DCS-induced and spontaneous SOZ was measured, and correlated with good (Engel I) and poor (Engel II-IV) outcome. We analyzed clinical variables which may be associated with a higher likelihood of inducing seizures during DCS: location of the SOZ, volume of the spontaneous SOZ, stimulation frequency (50 Hz or 1 Hz), spontaneous seizure-onset EEG pattern, and underlying pathology. Results: A total of 103 patients (49 men; 44 with Engel I outcome) were included. At least one ‘habitual’ electroclinical seizure was induced in 57 patients (55 %). DCS at 1 Hz induced events in 12 patients, whereas DCS at 50 Hz in 54 patients. The percentage of resection of DCS-induced SOZ was 27 % in the good outcome versus 11 % in the poor outcome group (p=0.003). Similar values were found for the spontaneous SOZ (29 % versus 11 %, p=0.002), as shown in Figure 2. The median of the percentage of agreement between both SOZs was 64 %. A stimulation frequency of 50 Hz rather than 1 Hz was the only variable associated with higher likelihood of eliciting seizures during DCS (p =0.002). Seven patients had only DCS-induced but no spontaneous seizures. There was no significant difference in the percentage of good outcome between these patients (4/7, 57%) and the whole group (42 %; p=0.35). Conclusions: We demonstrated in a large, two-center cohort that ‘habitual’ electroclinical seizures can be induced in 55 % of patients. Resecting a higher fraction of the volumes of the DCS-induced SOZ led to a better surgical outcome; this was similar for the spontaneous SOZ. Our data suggests that early use of DCS during implantation could result in a substantially reduced duration for S-EEG evaluation. Funding: This work was supported by the Canadian Institute of Health Research (grant FDN-143208 to J.G.). B.F.’s salary is supported by a salary award (“Chercheur-boursier clinicien Junior 2”) 2018 – 2021 of the Fonds de la Recherche en Santé du Québec.
.tmb-.png?Culture=en&sfvrsn=95643d05_0)