Subjective vs Objective Monitoring to Assess The Efficacy of Steady State Closed-Loop Neurostimulation Systems in Treating Medically Refractory Epilepsy
Abstract number :
1.452
Submission category :
4. Clinical Epilepsy / 4C. Clinical Treatments
Year :
2018
Submission ID :
538620
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Dorris D. Luong, Kaiser Permanente Sacramento Center and Ning Zhong, Kaiser Permanente Sacramento Medical Center
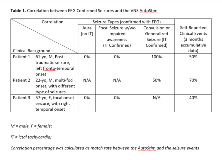
Rationale: Neurostimulation is an increasingly accepted treatment strategy for patients with medically refractory epilepsy. Closed-loop, on demand neuro-stimulation systems modulate/adapt therapy in response to neural or physiological changes, which may provide more effective and efficient therapy. Responsive neurostimulation (RNS) is activated by electrocorticography (EcoG) patterns. The vagus nerve stimulator AspireSR 106 (VNS) is also a closed-loop device, of which autostimulation (AutoStim) is triggered by detection of ictal tachycardia (IT). Clinical data are available to link long-term ambulatory EcoG data to the subjective seizure awareness in RNS-implanted patients. However, there was no study reporting the correlation between objective data (extended EEG recording) and the triggered AutoStim in patients with VNS during long-term follow up. We explored the association between objective seizure detection by continuous EEG (cEEG) or ambulatory EcoG, the responsive stimulation, and the subjective report. Methods: Data was collected at least 12 months post device implantation, when the stimulation parameters reached targeted therapeutic level and steady state. Time stamp data of VNS AutoStim were retrieved, the interrelated EcoG or cEEG during the same interval were acquired. The correlation between seizure detection and RNS stimulation, between seizure detection and VNS Autostim were analyzed. Results: All the patients reported benefits from the stimulator therapy with reduced seizure frequency and/or severity. 1) RNS and VNS was compared head-to-head in a patient (40 yo, F, bitemporal onset) with both RNS/VNS devices. The long term ambulatory EcoG data was strongly correlated (over 90%) with the self-reported seizures. VNS AutoStim was delivered 1/3 of the time when patient had clinical events. RNS also detected ictal patterns when no clinical events reported, and RNS stimulation were successfully delivered, which terminated the electrographic seizures. VNS AutoStim was delivered in only 3 out of total 24 such electrographic seizures. 2) Separate group patients with only VNS were monitored with cEEG for 5 days. The correlation between the AutoStim with EEG-confirmed clinical or electrographic seizures were not as robust as expected (Table 1). Intriguingly, during the outpatient clinic follow-up, the association rate was higher; over 50% between the AutoStim and the patient self-reported events. 3) High false-positive rate of AutoStim was also noted while during the monitoring or outpatient follow-up. Over 80% of the AutoStim were without association of seizure events. There was poor association between hourly/daily AutoStim rate and the seizure detected by either ambulatory EcoG or cEEG (Figure 1). Conclusions: The RNS ambulatory EcoG data highly correlates with the self-reported clinical events and is also sensitive to detect electrographic seizures. The RNS EcoG can reliably be used as seizure detection and assessment of seizure control efficacy. VNS AutoStim may deliver therapeutic stimulation when affirmative IT is detected. However, the association rate was not robust when examining the objective data, when compared to the self-reported events. Unlike the RNS average ictal activity pattern, the VNS daily AutoStim rate has less indicative value for seizure management. Using daily average AutoStim rate as a seizure detection biomarker should be further tested. Funding: No
.tmb-.png?Culture=en&sfvrsn=ce4bc4bf_0)