Surgery for Epilepsy in the Setting of Polymicrogyria: Cleveland Clinic Experience
Abstract number :
1.365
Submission category :
9. Surgery / 9C. All Ages
Year :
2018
Submission ID :
501743
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Aung Thandar, Cleveland Clinic; Juan Bulacio, Cleveland Clinic; Bo Jin, School of Medicine, Zhejiang University; William Bingaman, Cleveland Clinic; Jorge A. Gonzalez-Martinez, Epilepsy Center, Neurological Institute, Cleveland Clinic; and Imad M. Najm, C
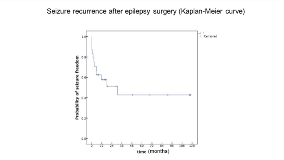
Rationale: Polymicrogyria(PMG) is a post-migrational malformation of cortical development and incidence of epilepsy is reported up to 65%-87%. Most patients with PMG related epilepsy have childhood onset, which becomes frequently refractory to medical treatment. According to Cossu et al, surgery is superior to medical management for achieving seizure freedom in PMG related epilepsy. In addition, according to recent publication Maillard et al, epileptogenic zone in PMG is heterogeneous and may be unrelated or extend far beyond the PMG cortex. In this study, we would like to compare the seizure outcome in PMG-related epilepsy patients who underwent medical management, patients who underwent straight resection without invasive intracranial EEG monitoring, and patients with medical management. Also, we also study the role of the extent of the lesion (unilateral vs bilateral) in relation to seizure freedom and epileptogenic zone in relation to the MRI lesion. Methods: Retrospective study conducted under Cleveland Clinic IRB. Patients with PMG related epilepsy admitted to Cleveland Clinic Epilepsy monitoring unit from 2001 to 2017, are enrolled. Patient without PMG, patient with PMG associated with hemimegalencephaly and patient who had an inconclusive evaluation were excluded. Epileptogenic zone (EZ) is defined as ictal onset zone in intracranial EEG. Seizure freedom is defined as no seizure recurrence at last follow up. Results: Total of Thirty-six PMG-related epilepsy patients were enrolled in the study with 2-167 months follow up duration (Mean 40 months and Median 18 months). Of those, 24 patients underwent surgery. 50% (12 patients) of surgical group became seizure free with 8-118 months follow up duration (Mean 45 months, Median 23 months). None of the patient became seizure free in non-surgical group (12 patients). 16 out of 24 patients in surgical group underwent invasive intracranial EEG monitoring (11 sEEG, 5 SDG) and 8 underwent straight extensive resection. 6 patients (55%) from sEEG group achieved seizure free but only one (20%) out of 5 sDG patients became seizure free. In non-invasive surgical group, only 5 out of 8 patients (62%) became seizure free. 7 out of 8 patients in non-invasive surgical group were young (less than 8 year old at the time of surgery) and 7 out of 8 patients had unilateral PMG. In regards to the extent of MRI lesion, 16 patient from surgical group had unilateral PMG and 9 patients (56%) became seizure free. 8 patients had bilateral PMG and 3 (38%) achieved seizure freedom. In regards to invasive monitoring, 20 patients underwent invasive intracranial monitoring and 16 patients underwent surgery. In 8 patients, EZ is found only in the PMG. In 9 patients, EZ is extended and involved part of the PMG and non PMG regions. In 3 patients, EZ is found in the non-PMG region. Conclusions: Surgical treatment has been so far underutilized in patients due to the extent of the malformations (often bilateral, multilobar, or diffuse and the presence of functionally critical cortex within the lesion. With current literature, epilepsy surgery seems to be the better treatment in patients with PMG and EZ may or may not overlap PMG. Focal resection may result in a favorable seizure outcome, even in cases of an extensive malformation Funding: None