Treatment and Outcomes After Stereoencephalography: Initial Experience at a Large-Volume Epilepsy Center
Abstract number :
1.226
Submission category :
4. Clinical Epilepsy / 4C. Clinical Treatments
Year :
2018
Submission ID :
499617
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Nicole Bentley, Emory University; Rohan Gupta, Emory University; Jon T. Willie, Emory University; and Robert E. Gross, Emory University
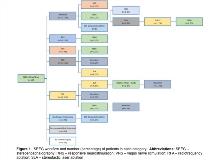
Rationale: Patients diagnosed with medically refractory epilepsy often require invasive intracranial monitoring to localize and treat epileptogenic zone networks (EZNs) responsible for initiating seizures. The stereoelectroencephalography (SEEG) approach, using stereotactically placed depth electrodes, enables recordings from superficial and deep cerebral structures, and can be effective in discriminating the EZN from propagation and/or uninvolved networks. Highly individualized neurosurgical techniques can then be considered to remove or modulate the EZN. Our institution adopted the SEEG approach 5 years ago, and our aim is to present surgical outcomes for subsequent consecutive patients that underwent SEEG at our institution. Methods: All patients that underwent SEEG from November 2012 to September 2017 were included in this study. A retrospective chart review identified cohort characteristics, neurosurgical management, and seizure outcomes. The Engel Outcome Scale was used to classify patients having >12-months follow-up. Patients were described as “seizure-free” or “not-seizure free” with respect to disabling seizures if they had <12-month follow-up. Descriptive statistics are provided with standard deviations (S.D.). Results: A total of 109 consecutive patients were included in the study, with a mean age at implantation of 36 ± 12 (range 17-66) years. Of these, 67% of patients were “lesional”, with an abnormality seen on MRI; the remaining were MRI-normal. Sixty-eight percent of patients underwent a successful initial implantation (mean length of stay [LOS] 10 ± 6 days), whereas 30% of patients underwent implantation of additional electrodes to aid localization (mean LOS 23 ± 11 days). Seizure onsets were unilateral in 80%, bilateral in 11%, and unidentifiable in 9%. The lobes identified as the EZN were unilateral temporal (46%), frontal (17%), bilateral temporal (10%), parietal (2%), occipital (2%), and insular (1%); multi-focal EZN were found in 13%. Overall, mesial temporal lobe epilepsy (MTLE) was diagnosed in 51%. Regarding management, 94 patients (86%) underwent further surgical treatment (Figure 1), and surgery was recommended to 6 patients (6%) who remained undecided. 9 patients (8%) were not offered additional surgery. Overall major complication rate was 2% (1 hemorrhage, 1 delayed pulmonary embolus resulting in death). Of the patients that underwent surgical management, 41% were seizure-free or Engel class I (free of disabling seizures; SF/EI) at last follow up (Figure 2), with a SF/EI rate in the ablation/resection group (RFA/SLA/resection, n=64) of 55%, and 17% in the neuromodulation group (RNS/VNS, n=30). Overall, SF/EI rates by lobe were 38% (unilateral temporal, n=50), 18% (bilateral temporal, n=11), 61% (frontal, n=18), 100% (parietal, n=2), 50% (occipital, n=2), 0% (insula, n=1), 36% (multi-lobar, n=14), and 18% (no clear focus, n=11). Conclusions: SEEG is an effective technique for reliably identifying the EZN in patients with medically refractory epilepsy. Results of SEEG may then be used to guide individualized therapies, including resective, ablative, and neuromodulatory techniques, to attain seizure freedom. Seizure outcomes vary by lobe and technique used. Funding: Not applicable
.tmb-.jpg?Culture=en&sfvrsn=b1862f50_0)