Use of Single Pulse Electrical Stimulation to Identify the Seizure Onset Zone
Abstract number :
2.443
Submission category :
18. Case Studies
Year :
2018
Submission ID :
502194
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Dalila Lewis, Johns Hopkins Hospital and Joon-yi Kang, Johns Hopkins Hospital
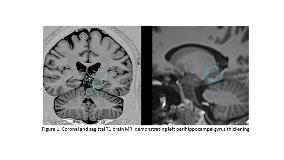
Rationale: Laser ablation is predominantly used for TLE associated with MTS. Dominant hemisphere MTS seems particularly amenable to ablation as it is a less invasive option with potentially less risk for post-operative cognitive or memory deficits.1 Seizure freedom rates are reported to be ~ 50-60%, and recent studies have shown that ablation can be used for lesions other than MTS. 2 This case highlights a unique case in which a good surgical outcome occurred following ablation utilizing single pulse electrical stimulation (SPES) following s-EEG implantation to assist in identification of the seizure onset zone (SOZ) in a patient with non-MTS TLE. Methods: A 38 year old right handed man with drug-resistant TLE having focal unaware seizures occurring twice weekly presented for presurgical evaluation. Semiology consisted of deja vu followed by unresponsiveness and confusion with occasional lip smacking. Brain MRI demonstrated mild asymmetric thickening in the dorsal left perihippocampal gyrus, suspicious for cortical dysplasia (figure 1). Phase I presurgical evaluation yielded 8 typical seizures, demonstrating a left temporal ictal onset zone that was maximal over the left anterior to mid-temporal regions. Subsequent phase II presurgical evaluation with 3 depth electrodes and 4 strips yielded 3 typical seizures, originating from depth electrodes simultaneously in the perihippocampal gyrus thickening and amygdala. Single pulse electrical stimulation (SPES) was conducted through a pair of adjacent electrodes: monophasic, alternating polarity, square wave pulse with pulse width of 0.3 ms at fixed frequency of 0.2 Hz, average of 50 trials/electrode pair. Stimulation of LDD depth electrodes at 0.5 mA produced a typical seizure. Evoked potentials demonstrated directional effective connectivity; stimulation of the perihippocampal gyrus thickening evoked responses in amygdala contacts while stimulation of the amygdala evoked a localized response only (figure 2). Based on the s-EEG and SPES, we hypothesized that the perihippocampal gyrus rather than the amygdala was the critical component of the SOZ. Results: The patient underwent ablation of the perihippocampal gyrus thickening without adverse events. He is seizure free at six months post-surgical follow-up. Conclusions: This case illustrates a unique method for identifying, verifying, and targeting a non-MTS seizure focus using SPES during pre-surgical evaluation. Although SPES is commonly used to identify functional networks, little is known about using SPES to understand seizure networks.3 Information regarding directionality from effective connectivity was critical in determining the ablation target. SPES resulted in a habitual seizure in this case and verified the SOZ. We propose that SPES may enhance current presurgical evaluation by providing directional information regarding ictal propagation and aid in identification of the SOZ. Funding: None
.tmb-.jpg?Culture=en&sfvrsn=be44b36d_0)