Utility of Salzburg Consensus Criteria for Nonconvulsive Status Epilepticus and Amplitude-Integrated Electroencephalography for Monitoring Electroencephalography of Patients With Refractory Status Epilepticus
Abstract number :
2.020
Submission category :
3. Neurophysiology / 3B. ICU EEG
Year :
2018
Submission ID :
501715
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Hyun-Woo Kim, Asan Medical Center; Hyo Jae Kim, Asan Medical Center; Sang-Ahm Lee, Asan Medical Center; and Yong Seo Koo, Asan Medical Center
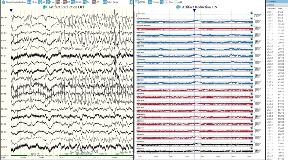
Rationale: Electroencephalography (EEG) monitoring is necessary to treat electrographic seizure in patients with refractory status epilepticus (RSE). To diagnose non-convulsive status epilepticus, Salzburg consensus criteria for diagnosing non-convulsive status epilepticus (SCNC) is currently considered as a gold standard. Quantitative EEG such as amplitude-integrated EEG (aEEG) not only has reasonable diagnostic accuracy, but also is easy and quick to review. The aim of the present study was to assess the utility of SCNC and aEEG as monitoring tools for patients with RSE. Methods: We selected 11 patients with RSE who underwent 24 hr EEG monitoring at Asan Medical Center. For patients with more than 48 h of EEG, only the earliest 24 h of recordings were included. Two authors marked all point of seizures using modified SCNC without clinical information. One author, who did not have any information of raw EEG data, marked seizures using aEEG according to continuity and integrated voltage (>10 ?). EEG and aEEG were divided into 10s epochs, classified as either ‘seizure’ or ‘non-seizure’. Epochs labeled as ‘seizure’ were marked as having seizure for all 10s period. All other epochs were classified as ‘non-seizure’. We calculated interobserver agreement for SCNC and sensitivity and specificity for seizure identification using aEEG compared with SCNC. Results: We enrolled 11 patients (age 58.2 ± 16.5, men 55%) with RSE. The 11 EEG recordings contained 1,201 discrete seizures over 234 hours. Two readers showed high interobserver agreement for SCNC (kappa = 0.91). Sensitivities for seizure identification in aEEG based on Salzburg criteria were 35.4% (reader 1) and 34.7% (reader 2). But, specificities were 97.1% and 97.3%. Kappa for inter-rater agreement between readers and aEEG were both 0.40 (p<0.0000001). Conclusions: Our study showed very high interobserver agreement for modified SCNC, which suggest its usefulness in monitoring RSE patients. However, marking 10-s EEG epochs using modified SCNC is hard to implement in real clinical practice. Although low sensitivity of aEEG suggests its inability to catch all subtle seizures of RSE patients, high specificity of aEEG suggests its ability to identify severe seizures. Further studies are needed to establish whether treatment change in response to SCNC and aEEG monitoring affects clinical outcome. Funding: None
.tmb-.jpg?Culture=en&sfvrsn=cd570bf4_0)