Valacyclovir-Induced Cortical Myoclonus
Abstract number :
3.129
Submission category :
3. Neurophysiology / 3B. ICU EEG
Year :
2018
Submission ID :
507096
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Yamane Makke, Mayo Clinic and Jeffrey W. Britton, Mayo Clinic
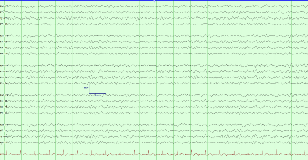
Rationale: Valacyclovir is the antiviral of choice for the treatment of herpes zoster. The dosing for patients with intact renal function is 1g three times daily. For patients on hemodialysis, the dose should not exceed 500 mg per 24 hours. The neurotoxicity secondary to valacyclovir was described predominantly manifesting as headache, altered awareness, hallucination in addition to reports of seizures and choreiform movements. We report a case of cortical myoclonus and generalized sharp waves with triphasic morphology in the setting of valacyclovir overdose in a patient on hemodialysis. Methods: 75-year-old woman with Lewy body dementia, left hemispheric ischemic infarct and end-stage renal disease on hemodialysis was evaluated for a rash over the left lower extremity and buttock that consisted with varicella zoster. Valacyclovir 1g three times daily was prescribed. Within two days of therapy, she developed a low grade fever (101 ° F) and altered mental status. During dialysis, she developed abnormal movements concerning for seizures. The patient was intubated and empirically started on vancomycin, amoxicillin, acyclovir, and ceftriaxone for concern of meningitis. She received 1 g of levetiracetam, an unclear dose of lorazepam, and valacyclovir was discontinued. The patient was then transferred for evaluation of her acute encephalopathy and presumed epileptic event. Her neurological exam was remarkable for grimacing and withdrawal to noxious stimuli, diffuse rigidity , and occasional arrhythmic jerking of distal upper extremities and feet, stimulus induced at times. She also had an upgoing toe on the right. Her CT head was unremarkable for any acute pathology. EKG was unremarkable. Urinalysis was positive for pyuria and bacteriuria. Electrolytes were unremarkable except for creatinine 6, BUN 38, and CBC showed mild anemia. She had a lumbar puncture which showed a high white cell count of 28, predominantly lymphocytic with 13 RBC, protein 99 and glucose 46. Results: Prolonged video EEG monitoring showed diffuse 3 to 5 Hz slowing with occasional emergence of an 8 Hz alpha PDR. This progressed to nearly continuous multifocal and generalized sharp triphasic complexes by the second day of the recording. Occasionally, sporadic episodes of cortical myoclonus occurred in association with generalized sharp waves with triphasic morphology on EEG (Figure 1). Other body movements also occurred without EEG correlate. Given the likely diagnosis and patient’s fragile status, aggressive anticonvulsant or sedative therapies were not administered. Myoclonus and mental status improved to baseline within 48 hours of valacyclovir discontinuance, and follow-up EEG was improved with complete resolution of the generalized discharges with triphasic morphology and of the myoclonic jerks (Figure 2). Conclusions: Valacyclovir has been previously reported to produce encephalopathy. The resolution of the patient’s EEG abnormalities and encephalopathy after discontinuation of valacyclovir would be consistent with an encephalopathy induced by this agent. The EEG findings were consistent with an encephalopathy, but the frequent periodic discharges were concerning for non-convulsive status epilepticus. However, considering the likely etiology, removal of the probable offending agent was decided to be the most appropriate management direction in this patient. Funding: None