Vigabatrin in the Treatment of Refractory Malignant Migrating Partial Seizures in Infancy - A Case Report
Abstract number :
2.143
Submission category :
4. Clinical Epilepsy / 4C. Clinical Treatments
Year :
2018
Submission ID :
501944
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Paul Maertens, University of South Alabama and James Rini, University of South Alabama
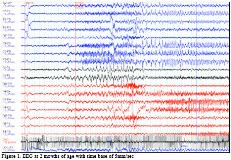
Rationale: The syndrome of malignant migrating partial seizures of infancy (MMPSI) or Coppola-Dulac syndrome is a rare devastating pharmaco-resistant epileptic encephalopathy characterized by onset within the first 6 months of life, progressive increase in seizure frequency, clusters of migrating electroclinical multifocal ictal patterns with independent bilateral hemispheric involvement and permanent deterioration of the psychomotor abilities. No effective treatment has been identified. The majority of cases are sporadic with several gene mutations having been reported by different groups such as SCN1A, PLCB1, and KCNT1. We report our experience with a 10-month-old Caucasian male with a history of malignant migrating partial seizure of infancy due to KCNT1 mutation. Methods: N/A Results: Our patient first developed seizures characterized by episodic 10-second bouts of forward extension of right arm followed by shaking at three days of life. Initial routine EEG at 10-days of life was normal however video-EEG monitoring at 3 weeks of age revealed focal spike-wave activity arising from C3 region. After one week of seizure freedom on levetiracetam, patient developed status-epilepticus requiring further evaluation. Extensive work up excluded metabolic and/or structural abnormality.By 3 month of age, he had regressed losing eye contact, vocalizing less spontaneously, becoming hypotonic and encephalopathic. Repeated interictal EEGs demonstrated multifocal independent spikes and polyspikes as well as disorganization of background activity. Patient subsequently failed multiple antiepileptic medication regiments including levetiracetam, phenobarbital, topiramate, oxcarbazepine, clonazepam, lacosamide and ketogenic diet. Eventually the child would fulfill the electroclinical criteria for MMPSI and a KCNT1 mutation was confirmed during genetic sequencing.By 5 months of age, patient had attempted quinidine, potassium bromide, cannabidiol, clobazam, felbamate, and ethosuximide however none of these antiepileptic regiments decreased seizure frequency. By 7 months of age, antiepileptic polypharmacy with quinidine, felbamate, clobazam and the recent addition of brivaracetam had failed with family reporting 20-30 clusters of seizures per day each seizure lasting 1-2 minutes in duration. At 8 months of age, the addition of vigabatrin immediately achieved a complete termination of electroclinical activity which has persisted allowing for a simplified drug regimen. By 10 months of age, he has begun to show signs of encephalopathic recovery; he is more alert, less irritable and vocalizes spontaneously. Conclusions: The majority of patients with MMPSI are refractory to conventional antiepileptic therapy. Case reports and case series have shown variable satisfactory to sustained response to certain antiepileptic regiments which include potassium bromide, levetiracetam, adrenocorticotropic hormone, stiripentol, clonazepam, quinidine, cannabidiol, and rufinamide. This report is the first to show support for the role of vigabatrin in the treatment of MMPSI and the possibility of complete sustained seizure control in this epileptic syndrome. Funding: Not applicable
.tmb-.jpg?Culture=en&sfvrsn=8ee889a8_0)