Do Functional Networks Evolve After TLE Surgery?
Abstract number :
1.259
Submission category :
5. Neuro Imaging / 5B. Functional Imaging
Year :
2018
Submission ID :
496214
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Bassel Abou-Khalil, Vanderbilt University Medical Center; Hernan F.J. Gonzalez, Vanderbilt University; Sarah Goodale, Vanderbilt University Medical Center; and Dario Englot, Vanderbilt University Medical Center
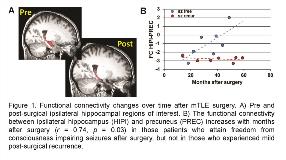
Rationale: Surgical treatment outcomes in mesial temporal lobe epilepsy (mTLE) remain variable and difficult to predict. We recently presented a presurgical mTLE connectivity network for distinguishing patients that will have a poor outcome (Engel III-IV) from those that will have some improvement (Engel I-II) after surgery.1 Here we probed this network pre and post-surgery to identify network characteristics related to freedom from consciousness impairing seizures vs. late mild recurrence after surgery as a means to improve specificity of prediction and understand recurrence mechanisms. Methods: We enrolled 15 mTLE patients for 3T functional MRI scanning (TR=2 s, 3x3x4 mm3, 600 vols) before and after (mean ± stdev: 25.4 ± 14.7 months) mTLE surgery (Figure 1A) and 44 age and gender matched healthy controls. Patients were classified into two groups based on whether they attained freedom from consciousness impairing seizures (Engel Ia-b) after surgery (n=8), or those that experienced mild seizures (Engel Ic-II) prior to follow-up (n=7). We focused on three regions as part of the seizure propagation network: ipsilateral hippocampus (HipI), contralateral hippocampus (HipC) and the bilateral precuneus (Prec). Functional connectivity (FC) was computed as the correlation of pairwise regional time series, and normalized to standard deviations from age matched control by linear fit across the healthy control subjects. Pre and post-surgical FC were investigated to identify connectivity characteristics that are associated with seizure outcome. Results: In the presurgical data, when all the patients were experiencing seizures, the FC between HipI-Prec and HipI-HipC were less than age matched control (i.e. less than zero) (n=15, p < 0.001). This suggests that decreases in FC in these paths facilitate presurgical seizures. In the group of patients that had post-surgical seizure recurrence, the FC between the HipC-Prec was also impaired (FC < 0, p < 0.05). This pattern of impairment remained after surgery (FC < 0, p < 0.05).In the group of patients who became seizure free after surgery, the FC between the HipI-HipC remained impaired after surgery, but the FC between the HipI-Prec positively increased with the number of months after surgery (r = 0.74, p = 0.03) (Figure 1B). This increase in FC over time may indicate reorganization towards normalization of this connectivity occurring only in those whose were seizure free at the time of rescan. Conclusions: In this work we have presented preliminary evidence that post-surgical ipsilateral networks (specifically HipI-Prec) do evolve after surgery towards a more normal state only in those patients that will attain seizure freedom, while the same network remains impaired in those with mild seizure recurrence (Figure 2). The study is limited by the small sample size and the fact that post-surgical data are cross-sectional. However, the differences between the outcome groups are striking, and warrant further investigation as potential predictors of outcome and mechanisms for recurrence.[1] Morgan VL, et al. Epilepsia 2017. Funding: NIH R01 NS75270 (VLM); NIH R00 NS097618 (DJE)
.tmb-.jpg?Culture=en&sfvrsn=a547b17f_0)