Intermittent Idiopathic Atrioventricular Heart Block Masquerading as Seizure
Abstract number :
2.430
Submission category :
18. Case Studies
Year :
2018
Submission ID :
501253
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Nathan T. Cohen, Children's National Health System and John M. Schreiber, Children’s National Medical Center
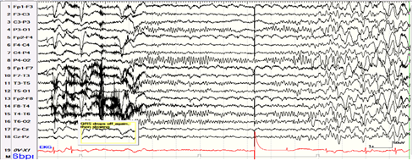
Rationale: Paroxysmal alterations of consciousness can be neurological in origin; however, a high index of suspicion is required to safely and correctly identify seizure mimics. Concomitant EKG monitoring and/or telemetry are important to correctly diagnose episodes due to arrhythmia. Here we present a teenage patient who was admitted to the inpatient neurology unit after initial emergency room evaluation with a provisional diagnosis of seizure or psychogenic non-epileptic seizure, who was subsequently found to have episodic asystole from intermittent idiopathic atrioventricular block on video EEG requiring pacemaker placement. Methods: A 17-year-old girl with a history of depression treated with escitalopram and intermittent polysubstance use (marijuana and alcohol) presented with a several day history of episodic sudden-onset altered mental status. She described a premonitory rising sensation in the chest and hallucinations of people ”talking and saying her name” and visual hallucinations of “an orange cat,” followed by a feeling of being “sucked out” of her body lasting up to 30 seconds. She would lose muscle tone during the events but had no tonic or clonic movements. She initially presented to an outside hospital emergency room where CBC, CMP, urinalysis and urine drug screen were negative. Head CT was normal. EKG showed normal sinus rhythm. Neurological and cardiac examinations were normal. After admission, she was placed on continuous video EEG monitoring with single lead EKG. This showed prolonged periods of asystole lasting 5-25 seconds, with irregular diffuse EEG background slowing appearing several seconds after the onset of asystole, and without focal or epileptiform activity. These changes were associated with her typical clinical events that prompted admission. The neurology team immediately transferred the patient to the cardiac intensive care unit. Repeat EKG showed normal sinus rhythm and an echocardiogram demonstrated normal structure and function. Ultimately, the patient received a dual chamber Medtronic pacemaker with resolution of her spells. Results: We demonstrate the successful identification and management of atypical complete heart block mimicking seizure. Except for the continuous video EEG with EKG lead, the diagnostic work-up was unrevealing including negative labs, EKG, head and cardiac imaging. Conclusions: This case demonstrates the need to maintain a high level of suspicion for alternative diagnoses in the work-up of seizure versus syncope. Typical evaluation for syncope was normal. Video EEG with single-lead EKG during episodes allowed for rapid diagnosis of complete heart block, and for safe and timely implantation of cardiac pacemaker. Funding: Not applicable