Long-Term, Durable Seizure Frequency Reduction in Individuals with CDKL5 Deficiency Disorder (CDD) Treated with Ganaxolone
Abstract number :
3.283
Submission category :
7. Antiepileptic Drugs / 7B. Clinical Trials
Year :
2018
Submission ID :
506062
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Nicola Specchio, Bambino Gesù Children Hospital; Lorianne Masuoka, Marinus Pharmaceuticals; Alex Aimetti, Marinus Pharmaceuticals; and Michael G. Chez, Sutter Neuroscience Institute
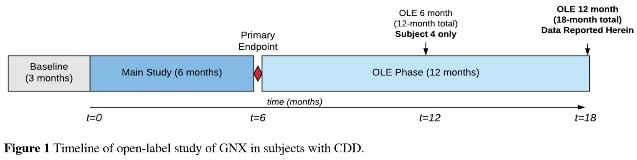
Rationale: Mutation of the cyclin-dependent kinase-like 5 (CDKL5) gene leads to early-onset treatment refractory seizures, gross motor impairment, and neurodevelopmental delay. Currently there are no approved drugs indicated for CDKL5 Deficiency Disorder (CDD). Existing antiepileptic drugs (AEDs) and ketogenic diet have demonstrated limited efficacy related to seizure burden and any benefits are typically short-lived. Müller et al. reported seizure response rates at 12-months that were one-third of the noted response rate at 3-months on a stable regimen of various AEDs signifying lack of long-term efficacy. There is a significant need for new antiepileptic drugs that reduce seizure frequency with safe and durable action.Ganaxolone (GNX) is an investigational drug that acts as a positive allosteric modulator of synaptic and extrasynaptic GABAA receptors and has known anticonvulsant activity. GNX was evaluated in an open-label study in individuals with CDD and 6-month primary endpoint seizure efficacy was previously reported. Here we report for the first time long-term data in a cohort of subjects that continued into the open-label extension portion of the study. Methods: Seven individuals with a confirmed mutation in the CDKL5 gene were enrolled and treated with oral GNX at doses up to 1,800 mg/day. The primary efficacy endpoint was defined as percent change in seizure frequency (all seizure types) per 28 days at 6-months relative to baseline (main study). Subjects that responded to GNX (n=4, seizure frequency reduction > 35 %) were enrolled in the open-label extension (OLE) phase for up to 1-year. Here we report 12-month data in the OLE phase (18-month total) for all subjects except one (12-month total data only). Percent change in seizure frequency in the OLE only includes seizure data in the OLE phase relative to baseline and does not include seizure data from the main study (Fig.1). Results: Four subjects were included in the OLE phase with a -54.1% (median) change in seizure frequency at the 6-month primary endpoint. To date, median seizure frequency for these subjects improved to -66.0%. One subject continued to experience a robust and durable seizure reduction (85-90%) and another subject dramatically improved from 6-months to 18-months (38% to 87% reduction). Two subjects noted mild increases in seizure frequency at 12 or 18-months relative to 6-months, yet both remain improved from baseline and demonstrate clinically meaningful seizure reductions (-37 to -45%) at or beyond 12 months (Fig.2). Conclusions: CDD is a recently recognized distinct clinical entity with significant unmet medical need. New drugs that effectively reduce seizures with durable action and that are well-tolerated are highly needed. GNX has demonstrated preliminary evidence of sustained, long-term efficacy in a small cohort of subjects. These findings are medically important since the durability of existing AEDs in this patient population is severely limited. Based on these encouraging data, the first global randomized, controlled pivotal study with GNX in children with CDD is scheduled to initiate in 2018 to further investigate the drug's effect. Funding: Marinus Pharmaceuticals
.tmb-.jpg?Culture=en&sfvrsn=d6b8e162_0)