Predictive Value of Early EEG in Neonates With Moderate Hypoxic-Ischemic Encephalopathy
Abstract number :
2.016
Submission category :
3. Neurophysiology / 3A. Video EEG Epilepsy-Monitoring
Year :
2018
Submission ID :
501830
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Alok Singla, John R Oishei Children’s Hospital, University at Buffalo; Mohamed Nasser, University at Buffalo - SUNY; Osman Farooq, University at Buffalo - SUNY; Sarah G. Finnegan, University at Buffalo - SUNY; Richard D. Thomas, John R Oishei Childr
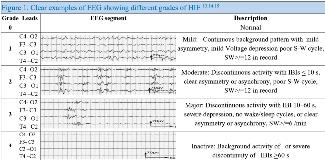
Rationale: Neonatal hypoxic-ischemic encephalopathy (HIE) remains a leading cause of newborn mortality & long-term morbidity. Therapeutic hypothermia (TH) is the first effective treatment for moderate to severe HIE. The aim of this study was to evaluate the positive predictive value (PPV) of early EEG (obtained within 6 hrs of life), APGAR score, Umbilical (U) cord pH & HIE severity as per Sarnat staging (stage I = mild, stage II =moderate) on MRI brain outcomes after TH & to investigate continuous video-EEG (CVEEG) features that could act as prognostic predictors for normal MRI. Methods: Retrospective analysis of all infants with gestation age GA =35 wks with moderate HIE treated with TH at Women & Children’s Hospital of Buffalo between September 2016 to December 2017 was done. Demographics & clinical data were collected as per study aims. Early EEG was graded (G) from 0 to 4 (Figure 1) based on the severity of background abnormalities (discontinuity, asymmetry, sleep-wake (S-W) cycle, interburst interval (IBIs), voltage depression (VD), & sharp waves (SW). Infants with severe HIE or clinical seizures at birth were excluded. Early EEG was analyzed for first 50-min, as well as the first 24 & 72 hrs of life. MRI obtained after TH was scored for HIE changes in basal ganglia, watershed (W) cortex & combined BG/W areas. MRI was graded mild ( W scores = 2) & moderate to severe (W scores = 3 or BG =2). PPV of early EEG for adverse MRI outcome and likelihood ratio (LR) were calculated. Results: 60 infants with mean GA of 39 + 2.3 wks & birth weight of 3.3 +1.3 kg with clinical mild or moderate HIE were identified. Nine infants with mild HIE (Sarnat stage I & normal EEG) were not cooled. Fifty-one of these (27 m, 23 f) underwent TH & were used for data analysis. The mean cord pH was 7.02 + 0.2 & median 5 & 10-min APGAR score was 5 & 7. TH was initiated within 3.5 + 2.2 hrs & early EEG was attained in 3.5 + 2.2 hrs of life. Forty-nine (96%) infants were Sarnat stage II & two (4%) were stage I with early EEG changes. Thirty-one (61%) infants with overall early EEG background abnormalities were graded moderate to severe (G 2,3 & 4) in twenty-four (77%). Infants with cord pH < 7.0 had 75% while cord pH >7.0 had 54% early EEG changes [p=.01]. Post TH MRI was done at the median age of 5 days [I QR=3,6]. MRI injuries were localized to a W cortex in eight, BG in one & BG/W areas in seven infants. 60% MRI injuries were mild & 40% were moderate to severe. 85% of infants with normal early EEG & 100% with stage I + abnormal early EEG had normal MRI after TH. The PPV of 10-min APGAR score < 5 for early EEG changes was 57% whereas NPV for adverse MRI outcomes was 100%. The PPV of early EEG for adverse MRI outcomes in infants with U cord pH < 7.0 was 20% [LR 2.1, 95% CI 1.3- 3.3]. PPV of overall abnormal early EEG was 22.5% [LR 1.3, 95% CI 0.8- 2.1] which increased significantly if early EEG background was moderate to severely (G 2,3 & 4) abnormal [PPV 25%, LR=2.1, 95% CI 1.3- 3.3]. During TH & rewarming, early EEG features were improved in 54% CVEEG. 27% had a reduction in IBIs & up to 38% had improved VD & S-W cycle differentiation. MRI was normal in 73% with VD & S-W cycle improvement & 38% abnormal with improved IBIs (Table 1). Conclusions: Our study suggests that early EEG abnormalities of grade 2 or higher are sensitive in detection of post TH MRI changes in moderate HIE. Also, early EEG was sensitive for abnormal MRI if U cord PH < 7. 0. Improvement of early EEG features such as VD & S-W cycle were good prognostic predictors for normal MRI. We conclude that early EEG grading can be a valuable tool in the decision making for selecting infants for TH when clinical parameters are not conclusive. Improvement in CVEEG features can be a valuable tool in predicting post-TH MRI changes. Funding: None
.tmb-.jpg?Culture=en&sfvrsn=52511a4e_0)