Short-Term Neurostimulation Trials During Invasive Monitoring of Epilepsy Patients
Abstract number :
3.154
Submission category :
3. Neurophysiology / 3E. Brain Stimulation
Year :
2018
Submission ID :
507446
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Nicholas M. Gregg, Mayo Clinic; Anthony L. Fine, Mayo Clinic; Igor A. Lavrov, Mayo Clinic; Katherine C. Nickels, Mayo Clinic; Eric T. Payne, Mayo Clinic; and Brian N. Lundstrom, Mayo Clinic
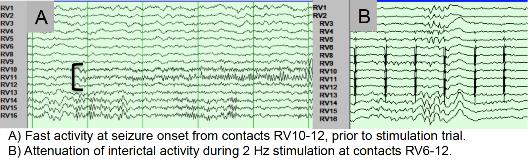
Rationale: Neurostimulation trials during invasive monitoring for epilepsy surgery may provide information to help guide patient selection and stimulation targets for chronic neurostimulation. Stimulation during monitoring allows simultaneous assessment of interictal activity, seizure frequency and onset pattern. Two patients recently underwent neurostimulation trials at our institution. Methods: E is a 16-year-old cognitively normal right-handed young lady with intractable epilepsy and extensive bilateral perisylvian polymicrogyria, maximal on the right hemisphere. Seizures are typified by a “fuzzy feeling,” with or without impaired awareness, and left arm weakness, occurring weekly. Prior EMU evaluation localized seizures to the midline and right central region, and ictal-SPECT and MEG localized the onset to right polymicrogyria regions (fMRI hand motor area). E underwent stereo EEG monitoring of right perisylvian and insular regions. A trial of neurostimulation of the seizure onset zone (SOZ) was performed using a Medtronic Test Stimulator (biphasic pulses, 2-100 Hz, pulse width 90-450 µs, and 1-6 V).T is a 17-year-old right-handed young man with intractable epilepsy and daily seizures. Imaging is notable for an asymmetrically small left hippocampus. His seizure semiologies are 1) impaired responsiveness with purposeless walking (weekly), 2) myoclonic jerk with tonic arm posturing, max right (daily), and 3) GTCs (none past year). EEG and ictal SPECT localized seizures to the left inferior frontal/frontotemporal regions. T underwent stereo EEG monitoring of the left frontal and temporal regions. A trial of neurostimulation was completed. Results: While on reduced medications, E was stimulated through 14 contacts from 3 leads involved in the SOZ, most often with parameters of 2 Hz, 1 V, and 300 µs pulse width. E had attenuation of interictal activity at stimulated contacts (fig. 1), and no seizures during 48 hours of stimulation; 2 seizures occurred within 1 hour of stimulation discontinuation. She underwent implantation for Chronic Subthreshold Cortical Stimulation (Lundstrom B, et al., JAMA Neurology, Nov. 2016, Vol. 73 Num. 11 pg 1370-1372) in April, 2018, stimulation was started 3 weeks later, and stimulation adjustments are ongoing.T had diffuse seizure onset, and an unsuccessful stimulation trial with continued frequent interictal activity and seizures during monitoring. He was deemed a poor candidate for neurostimulation due to diffuse SOZ and unsuccessful stimulation trial. Conclusions: Neurostiulation trials during invasive EEG monitoring for epilepsy surgery may provide information to help guide decisions on candidacy for chronic neurostimulation, and direct neurostimulation targets. More work is needed to determine the predictive value of neurostimulation trials with regard to the efficacy of permanent neurostimulation implants. Risks of neurostimulation include prolonged time in the ICU, and risk of precipitating seizures. Funding: No relevant funding