9.4 T MRI CHARACTERIZATION OF A FOCAL LESION IN THE RAT BRAIN INDUCED BY INTERLACED MICROBEAM RADIATION
Abstract number :
3.019
Submission category :
Year :
2005
Submission ID :
5825
Source :
www.aesnet.org
Presentation date :
12/3/2005 12:00:00 AM
Published date :
Dec 2, 2005, 06:00 AM
Authors :
1,2David J. Anschel, 2Bernd Foerster, 3Tetsuya Yuasa, 2,4Helene Benveniste, 5Zhong Zhong, 2James Hainfeld, and 2Avraham Dilmanian
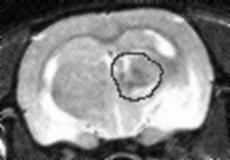
The use of radiosurgery to non-invasively treat epileptic foci is currently an active topic of clinical and preclinical research. Modalities such as proton beams, Gamma Knife and Cyber Knife have allowed for some recent advances over the traditional linear accelerator. A primary limitation of these techniques remains unwanted damage to brain and other tissues outside of the targeted area. We report the use of parallel x-ray microplanar beams in an [quot]interlaced[quot] geometry to deliver a dose to a 3.8 x 3.8 x 3.8 mm3 region of the rat[apos]s cerebrum. It has been established that arrays of parallel, synchrotron-generated x-ray microplanar beams (microbeams) spare normal tissue, including the CNS. Interlaced microbeams have the advantage, over conventional beams, of a) sparing the normal CNS outside the target, and b) having an extremely sharp dose fall off at the edge of the target volume. A normal rat brain was focally irradiated in vivo to study the method[apos]s efficacy in precisely necrotizing brain tissue. The rat was positioned vertically using a plastic stereotactic frame, and was irradiated with two orthogonal arrays of 1 mm beam thickness and 1.36 mm beam spacing on-center. The interlaced volumes width was 3.8 mm and its height was 3.7 mm (i.e. 3 microplanar beams in the array). The rat was irradiated superior-to- inferior and laterally with 100 Gy in-beam incident dose although one microplanar beam in the superior-to-inferior irradiation inadvertently delivered a higher dose. The rat was imaged using a 9.4 T MRI at regular intervals. The results show a gradually developing lesion at the site of the interlaced beams. The lesion began as a high T2 signal only, but advanced to include a central area of low T1 and T2 signal within 2 months. No lesion was observed in the other side of the brain which was exposed to non-interlaced microbeams only. Figure 1 shows a T2 weighted image taken 7 weeks post treatment. Interlaced MRT is an effective method to create focal brain microlesions. This technique may allow the future treatment of epileptic foci not accessible by surgical or more traditional radiosurgical means.[figure1] (Supported by NIH NINDS grant NS43231, Office of Biological and Environmental Research, U.S. Department of Energy.)