A Comparison of Psychological Characteristics of Psychogenic Nonepileptic Seizures and Epilepsy Patients Admitted to an Epilepsy Monitoring Unit
Abstract number :
2.223
Submission category :
6. Comorbidity (Somatic and Psychiatric)
Year :
2018
Submission ID :
502555
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Robin Garrett, Banner University Medical Center - Phoenix; Richard Gerkin, Banner University Medical Center - Phoenix; Steve S. Chung, Banner University Medical Center - Phoenix; Norman Wang, Banner University Medical Center - Phoenix; Hussam Seif-Eddeine
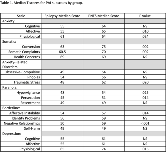
Rationale: Depression and anxiety are co-morbid in patients with epilepsy, and they may be emotional triggers for psychogenic nonepileptic seizures (PNES). Psychological assessment measures such as the Personality Assessment Inventory (PAI) are commonly used by neuropsychologists to assess for psychiatric disorders in this population. A prior study that compared PAI outcomes with epileptic and nonepileptic patients found elevations on the clinical scales sensitive to Somatic Complaints, Anxiety, Depression, Schizophrenia, and Borderline Features1. The purpose of our study was to further delineate psychological characteristics of epilepsy and PNES in an Epilepsy Monitoring Unit (EMU) population. Methods: Data were acquired via retrospective chart review of 55 patients presenting to an EMU over a one-year period. Females represented the majority (82.1%) of the PNES group (n= 28), while the Epilepsy group (n=27) was more equally distributed (59.3% female). For the total sample, gender, age, and years of education were not significantly different between groups. All patients completed the Personality Assessment Inventory (PAI) and the Beck Depression and Beck Anxiety Inventories (BDI-II and BAI) as part of a comprehensive neuropsychological evaluation. Results: Nonparametric tests (Mann-Whitney U) were performed to examine all between-group differences. No differences were found across any of the validity indicator scales. For Personality Assessment Inventory (PAI) Clinical Scales, patients with PNES had higher scores on the Paranoia (p=.031), Borderline Features (p=.007), Somatic Complaints (p=.014), Anxiety (p=.010), and Anxiety-Related Disorders (p=.020) scales. BAI scores were significantly higher in the PNES group (p=.009). Although there was a trend toward higher BDI-II scores and Depression PAI subscale scores in this group, this did not reach clinical significance. The table below includes exploratory analyses of subscales for clinical scales that were different between groups. Conclusions: The results confirmed prior findings that patients with PNES score higher on the following PAI clinical scales: Somatic Complaints, Anxiety, and Borderline Features. Our data also suggested the PNES group scored higher on PAI clinical scales Anxiety-Related Disorders and Paranoia. The finding of a higher score on the Anxiety-Related Disorders scale with a statistically significant elevation on the traumatic stress subscale is consistent with the literature that suggests trauma as a correlate of PNES2. Exploratory analysis of the subscales of the PAI are warranted to provide additional insight into psychiatric comorbidities in NES and epilepsy to develop effective treatment recommendations for an inpatient EMU population. References1Marc Testa S, Lesser RP, Krauss GL, Brandt J. Personality assessment inventory among patients with psychogenic seizures and those with epilepsy. Epilepsia. 2011;52(8);e84-e88.2 Kaplan MJ, Dwived AK, Privitera MD, Isaacs K, Hughes, C, Bowman M. Comparisons of childhood trauma, alexithymia, and defensive styles in patient with psychogenic non-epileptic seizures vs. epilepsy: Implications for the etiology of conversion disorder. Journal of Psychosomatic Research. 2013;75:142-146. Funding: Funding was not received in support of this abstract.