Anti-epileptic Drugs Reduce the Incidence of Cardiac Arrhythmias in Long QT Syndrome Patients
Abstract number :
3.396
Submission category :
Late Breaking
Year :
2015
Submission ID :
2409527
Source :
www.aesnet.org
Presentation date :
12/7/2015 12:00:00 AM
Published date :
Nov 23, 2015, 18:00 PM
Authors :
David S. Auerbach, Yitschak Biton, Bronislava Polonsky, Robert Gross4, 1, Robert T. Dirksen, Arthur Moss
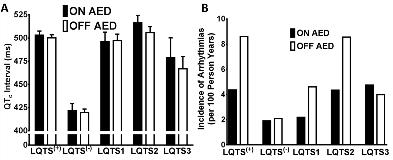
Rationale: Long QT Syndrome (LQTS) is a multisystem disease, and patients are at an increased risk of neuro-cardiac electrical disturbances. Genes that are altered in LQTS1-3 are expressed in both the heart and brain. Since many anti-epileptic drugs (AEDs) act upon ion channel activity (e.g. Na+ channel blockade, Ca2+ channel blockade, GABA agonists), we hypothesized that AEDs would also reduce the rate of cardiac arrhythmias in LQTS patients.Methods: Using the Rochester-based LQTS Registry, the study consisted of LQTS genotype (LQTS1-3) or phenotype (male QTc>450ms, female QTc>470ms) positive patients, termed LQTS(+) (n=310), and those genotype and phenotype negative, termed LQTS(-) (n=52). Sub-analysis of LQTS(+) patients included those genotype positive for LQTS1 (n=64), LQTS2 (n=84), and LQTS3 (n=15). All patients had a history of taking AEDs, and there were assessments of cardiac electrical function both on and off of AEDs. AEDs were classified as Na+ channel blockers, Ca2+ channel blockers, GABA agonists, and other mechanisms of action. Due to dual mechanisms of action some AEDs were classified in more than one group. Females comprised 71.6% of the LQTS(+) group and 76.9% of LQTS(-) group. Follow-up was from birth to 40 years of age (LQTS(+), 31.33±0.63; LQTS(-), 29.67±1.30 mean±SEM years follow-up). Outcome measures included QTc on the ECG and recurrent rate of cardiac arrhythmias. Comparisons were made on vs. off AEDs.Results: Among all LQTS(+), LQTS1, LQTS2, LQTS3, and LQTS(-) patients there was no difference in the mean QTc when patients were on vs. off AEDs (all p=ns, Figure 1A). In contrast, the event rate of cardiac arrhythmias per 100 person years of life was 2-fold lower in all LQTS(+) patients on vs. off AEDs (4.36 vs. 8.60, Figure 1B). Sub-analysis indicated that when LQTS1 and LQTS2 patients were on AEDs, there was also a 2-fold reduction in the event rate of cardiac arrhythmias when compared to off AEDs (LQTS1: 2.19 vs. 4.61; LQTS2: 4.34 vs. 8.55).Yet, AEDs were not associated with a reduction in the event rate of cardiac arrhythmias among LQTS(-) (1.90 vs. 2.09, on vs. off AEDs) or LQTS3 (4.75 vs. 3.98) patients. Interestingly, the rate of cardiac arrhythmias was reduced 1.42 and 2.70 fold when LQTS(+) patients were on vs. off GABA agonists (4.50 vs. 6.41, n=202) or Na+ channel blockers (4.33 vs. 11.67, n=236), with similar effects seen in LQTS1 and LQTS2 patients.Conclusions: The rate of cardiac arrhythmias was reduced when LQTS(+), specifically LQTS1 and LQTS2, patients were on vs. off AEDs. Yet the general anti-arrhythmic effect was not observed in either LQTS3 patients, who are at an increased risk of cardiac arrhythmias, or LQTS(-) patients. AEDs may exert anti-arrhythmic effects in LQTS(+) patients.