Comorbidities of Rare Epilepsies: Results From the Rare Epilepsy Network (REN)
Abstract number :
3.182
Submission category :
4. Clinical Epilepsy / 4A. Classification and Syndromes
Year :
2018
Submission ID :
506542
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Brandy E. Fureman, Epilepsy Foundation; Nhan T. Ho, Columbia University Medical Center; Barbara L. Kroner, RTI International; Kathleen Farrell, Epilepsy Foundation; and Dale C. Hesdorffer, Columbia University
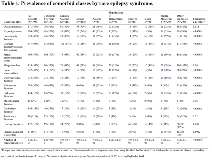
Rationale: Although many studies have examined epilepsy-associated comorbidities, very few studies have reported comorbidities in rare epilepsies. Despite being rare, these understudied conditions with epilepsy are associated with a broad spectrum of serious comorbidities and high mortalities. We describe prevalence and characteristics of a range of comorbidities across different groups of rare epilepsies. Methods: Persons with rare epilepsies and caregivers of affected persons were recruited through the Epilepsy Foundation and over 30 rare epilepsy advocacy organizations (REN). A web-based survey consisted of 12 core sections to collect data on the affected person’s demographics, seizure type, treatment, co-morbidities, development and behavior. Comorbidity information was grouped into 16 classes; each class had a broad Yes/No/Unsure stem question followed by detailed questions on specific disorders within the class. Participants with comorbidities involving two or more body systems were classified as having complex chronic disease (C-CD) and those without comorbidities or with comorbidities in one body system were classified as having noncomplex chronic disease (NC-CD). Validation of REN comorbidity information was done for Tuberous Sclerosis Complex (TSC), Aicardi and Phelan McDermid (PM) syndromes by comparing REN reported prevalence of representative comorbidities with that of reference cohort or literature. Results: Of 795 people with more than 30 different rare epilepsy diagnoses, half had =5 comorbidity classes and 85% were classified as having C-CD. The highest number of comorbidity classes reported per person were in patients with Aicardi, PM [median(interquartile range(IQR))= 7.0(5.0,9.0)] and TSC [median(IQR)= 6.0(4.0,8.0)]. The most common comorbidity classes were learning disability (65%), mental health issues (59%), sleep disorders (58%), oral issues (47%), brain abnormalities (43%), bone-joint issues (40%), hyper/hypotonia (37%), and eye-vision disorders (36%) (Table 1). The most medically complex syndromes were Aicardi, TSC, PM, Dup15q (%C-CD=100%, 97%, 97% and 90% respectively; Table 2). The prevalence of brain abnormalities, hyper/hypotonia, eye, and cardiac disorders was significantly higher in patients first diagnosed with epilepsy at younger age (<9 months old) compared to those first diagnosed at older age (trend p<0.05). Prevalence of main features for Aicardi and Phelan McDermid reported in REN were similar to those reported in the literature, although for TSC, prevalence of some features was higher in REN than in a reference cohort which included TSC with and without epilepsy. Conclusions: High number and high prevalence of many comorbidities were found in people with rare epilepsies, especially those who were first diagnosed with epilepsy at a younger age. A vast majority of people with rare epilepsies are medically complex. REN survey comorbidity information is consistent with previous reports. Our results emphasize that comorbidities should be attentively taken into account in the diagnosis and management of people with rare epilepsies. Funding: Funded by by the Patient-Centered Outcomes Research Institute (PCORI) (grant number PPRN-1306-04577) and the Mervyn Susser Fellowship in the Gertrude H. Sergievsky Center, Columbia University (to NTH).
.tmb-.png?Culture=en&sfvrsn=c42dc2df_0)