Complex Seizure Networks: Intracranial EEG Findings of Three Patients With Periventricular Nodular Heterotopias
Abstract number :
1.358
Submission category :
9. Surgery / 9B. Pediatrics
Year :
2018
Submission ID :
507284
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Julia Robinson, Children's Hospital Los Angeles; Matt Lallas, Children's Hospital Los Angeles; Andrew Kim, Children's Hospital Los Angeles; Michele Van Hirtum-Das, Children's Hospital Los Angeles; and Deborah Holder, Children's Hospital Los Angeles
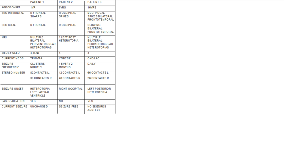
Rationale: Despite advancements in the treatment epilepsy, 30-35% of patients fail to achieve seizure control with standard treatment options. For these patients the best option is often surgery. Surgical candidates traditionally have focal seizures originating from a region considered safe to operate. Patients with periventricular nodular heterotopias (PVNH) had not previously met these criteria as their lesions had not been readily accessible to conventional resective surgical approach. With the advent of minimally invasive laser ablation (LITT) it became possible to access and ablate these deep lesions. First, in order to identify and map what we have discovered is often a complex network, stereo EEG is required prior to an attempt at laser ablation of a potentially epileptogenic nodular heterotopia. We present our initial experience with invasive monitoring of a group of patients with PVNH, followed by laser ablation when seizure onset could be attributed to the heterotopia. Methods: The Epilepsy Surgery Program at Children’s Hospital Los Angeles is a level IV epilepsy center serving Southern California. We reviewed our records since the start of minimally invasive laser ablation (LITT) and found three patients who underwent stereo EEG monitoring with PVNH. A chart review was obtained and will be reported here. Results: The demographic details of three identified patients are listed in chart 1. Patient one presented with infantile spasms at age 1 year and was treated initially with ACTH with resolution of spasms but continued with left focal body seizures. Video/EEG monitoring revealed right frontal sharp waves and slowing both interictally and ictally. MRI revealed multiple, bilateral PVNH and partial agenesis of the corpus callosum. A stereo EEG with multiple bilateral depth electrodes into all heterotopias as well surrounding cortex revealed two active heterotopias, left frontal and right posterior. The left frontal heterotopia was treated with laser ablation. Six months postoperatively, seizures have not significantly decreased but, the child interestingly has had a significant improvement in language and cognitive skills. Patient two had seizure onset at age 6 years. Scalp EEG demonstrated right posterior spikes both ictal and interictal and MRI revealed one heterotopia in the left lateral ventricle. Stereo EEG showed seizure onset in the right occipital cortex and no laser ablation ensued. Patient three had seizure onset at age 16 years. Multiple bilateral PVNH were evident on MRI and EEG revealed multifocal interictal spikes with diffuse ictal slowing over the bilateral frontotemporal regions with some suggestion of left anterior focus. Stereo EEG showed onset first in a left frontal heterotopia with rapid spread to a right posterior heterotopia and the left mesial temporal structures. Patient was treated with LITT of the left heterotopia. Conclusions: Minimally invasive laser ablation now offers physicians the option to treat PVNH in patients with drug resistant epilepsy. However, we have found the PVNH are not always the source of the seizures. These patients often have complex networks and require invasive monitoring prior to definitive treatment. A combination of treatments may be indicated to treat both the heterotopia and overlying cortex. Funding: Not applicable