Cost Analysis of Subdural Grids and Strips vs. Stereo-Electroencephalography in the Evaluation of Refractory Epilepsy
Abstract number :
2.340
Submission category :
9. Surgery / 9C. All Ages
Year :
2018
Submission ID :
507281
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Brian A. Tong, University of Texas Health Science Center; Miriam Morales-Morris, Mischer Neuroscience Institute; Jessica A. Johnson, University of Texas Health Science Center; Cristian Donos, University of Texas Health Science; Gretchen Von Allmen, McGove
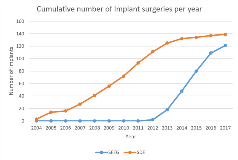
Rationale: The rapid adoption of stereo-electroencephalography (SEEG) relative to subdural electrodes (SDE), the current gold standard, has revolutionized the approach for intracranial evaluations of patients with non-lesional or ill-defined focal epilepsy in North America. The outcomes and complications of the two methodologies have been previously explored, but the direct costs associated with either method have not been extensively considered. In this study, the authors will compare the contribution margin and direct costs of these two approaches. Methods: Contribution margin and cost data from phase II monitoring and procedures performed by a single neurosurgeon on 260 patients from 2004 to 2017 were compiled through the Mischer Neuroscience Associates’ Innovation, Quality and Research Unit. Demographics, epilepsy characteristics, duration of monitoring, length of stay and procedural morbidity were all ascertained from a previously compiled database of the same patients from 2004 to 2017. Unpaired t-tests and chi-squared tests were performed to evaluate distinctions between the two groups. Results: Both SEEG (n=121) and SDE (n=139) groups were similar in age (30.1 ± 12.2 vs. 30.6 ± 13.8 years), gender (SEEG = 47.1% male; SDE = 43.9% male) and duration of epilepsy (16.4 ± 12.0 years vs.17.2 ± 12.1 years). The distribution of insurances among patients in the SDE cohort did not significantly differ from the distribution among patients in the SEEG cohort (p= 0.69). The duration of intracranial monitoring was comparable (SEEG = 7.7 ± 3.9 days vs. SDE = 8.1 ± 2.8 days). There were 7 symptomatic hemorrhagic sequelae and two infections in the SDE cohort with no clinical complications in the SEEG cohort (p = 0.004). Only one patient from the SDE cohort experienced long-term neurological sequelae related to the intracranial evaluation. A greater proportion of SDE patients underwent resective or ablative surgery (91.4%), compared with SEEG patients (72.7%, p < 0.0001). None of the SDE patients and 4.1% of SEEG patients underwent placement of the RNS device. 8.6% of SDE patients and 14.1% of SEEG patients were not thought to be candidates for further cranial intervention. The direct cost for SDE ($45,174.70 ± $11,162.43) was significantly lower than the value ($57,927.66 ± $17,383.01) for SEEG, including phase II monitoring and procedure, (p < 0.0001). The contribution margin for SDE ($68,314.83 ± $47,332.52) was lower than the value for SEEG ($79,005.24 ± $67,610.58), including phase II monitoring and procedure (p=0.14). In 2014, 2015 and 2016, the direct cost for SDE ($50,580.41 ± $6,073.32) was lower than the value for SEEG ($59,595.65 ± $12,760.52), including phase II monitoring and procedure (p=0.005). The contribution margin in those years for SDE ($77,209.59 ± $37,783.84) was higher than the value for SEEG ($71,967.19 ± $64,999.60), including phase II monitoring and procedure (p=0.748). Conclusions: Overall, the costs for SDE have been lower than those of SEEG from 2004 to 2017. However, the SDE cases have been concentrated in the beginning of the timespan, from 2004 – 2013, plateauing when SEEG was first implemented in the clinic from 2013 to present. To account for inflation, the direct costs and contribution margins were considered for 2014, 2015 and 2016. The direct costs and contribution margins were comparable during a short timespan, which indicates that inflation, around 3-5% per year, plays a role in the trends observed in costs and contribution margins. Funding: Not applicable