Diffusion Tensor Imaging Improves Assessment of Postoperative Interhemispheric Connections After Functional Hemispherectomy
Abstract number :
2.134
Submission category :
4. Clinical Epilepsy / 4C. Clinical Treatments
Year :
2018
Submission ID :
501371
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Mukesch Shah, University Medical Center Freiburg; Karl Egger, University Medical Center Freiburg; Marco Reisert, University Medical Center Freiburg; Alexandra Klotz, University Medical Center Freiburg; Peter Reinacher, University of Freiburg; Christian Sc
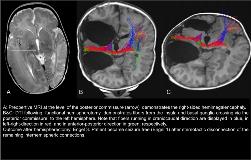
Rationale: Functional hemispherectomy can be used in patients with hemispheric lesions and medically intractable epilepsy. Success rates vary depending on etiology but rates of postoperative seizure freedom are between 50-70%. Thus hemispherotomy is the most promising treatment in these patients. In patients with remaining seizures after surgery it is often discussed whether these remaining seizures are still generated in the operated hemisphere and spreading via remaining commissures. Alternatively seizures might be generated by independent seizure foci in the contralateral hemisphere. In this project diffusion tensor imaging (DTI) was used to visualize and quantify interhemispheric connections pre- and postoperatively. Methods: Patients which received a functional hemispherectomy at the Freiburg Epilepsy Center underwent DTI (HARDI, >60 diffusion-encoding directions, 1.5×1.5×1.5mm3 voxels) directly prior and three months after their surgery. Postsurgical follow-up for seizure frequency was performed at 3, 6 and 12 months. DTI data were analyzed using an in-house software with a global tracking algorithm. Results: Between 2015 and 2017 15 patients underwent functional hemispherectomy and DTI measurements. 8 patients were seizure free. Four patients underwent pre and postsurgical DTI and 11 patients only postsurgical DTI. Out of the seven patients who continued to have seizures, in three EEG data suggested a seizure onset from the operated hemisphere. DTI revealed strong remaining connections via fibers of the anterior and posterior commissures (Figure 1). These connections were significantly stronger than in the seizure free patient group. Two patients received stereotactic ablation of the anterior and posterior commissures. One of them had reduced seizure frequency and the other was seizure free after this second intervention. Conclusions: Functional hemispherectomy are the most promising treatment for hemispheric refractory epilepsies. The current approach does not include a disconnection of the interhemispheric commissures. Our preliminary data suggests that some patients continue to have seizures via propagation from the operated hemisphere. In some patients with strong connectivity through these commissures a primary disconnection might therefore improve outcome. Secondary stereotactic ablation might be another well tolerated procedure. Funding: None