Electroclinical Features and Incidence of Generalized Paroxysmal Fast Activity (GPFA) in Children With Typical Absence Seizures
Abstract number :
1.149
Submission category :
3. Neurophysiology / 3C. Other Clinical EEG
Year :
2018
Submission ID :
495171
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Lalit Bansal, Children's Mercy Hospital; Lines Vargas, Children's Mercy Hospital; Kailash Pawar, Children's Mercy Hospital; Deepti Nagesh, Children's Mercy Hospital; Mohammed Ilyas, Children's Mercy Hospital; Ara Hall, Children's Mercy Hospital; Brad Kinn
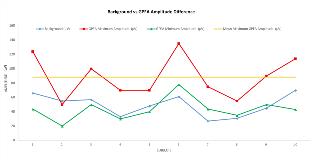
Rationale: Generalized paroxysmal fast activity (GPFA) is a diffuse, paroxysmal, frontal predominant activity described in patients with generalized epilepsies, epilepsy syndromes like Lennox-Gastaut syndrome (LGS), Jeavons syndrome and genetic generalized typical absence seizures (TAS) of adults. Studies specifically focusing on electro-clinical features of TAS in children have not reported any GPFA-like features, and the significance of GPFA on EEG is unclear. We sought to identify GPFA in children with TAS and study its incidence, characteristic electroclinical features, and effect on their epilepsy. Methods: We performed a retrospective review of EEGs of children with a diagnosis of absence epilepsy. A total of 173 subjects were identified. In subjects with GPFA on their EEGs, GPFA characteristics were collected (i.e. predominant location, duration, amplitude, frequency, provocation factors and if GPFA was followed by spike-wave discharges). In GPFA-positive subjects, further data sets were collected examining their demographics, duration of epilepsy, and pharmacoresponsiveness to epilepsy. Results: GPFA was identified in 10 subjects (5.78%) with a female-to-male ratio of 9:1. Median age of subjects was 17 years and median duration of illness was 9.5 years. Mean maximum GPFA amplitude was 88.3 µV (Fig. 1) with a posterior predominance in 9/10 subjects. GPFA frequency ranged between 11 and 20 Hz with a duration of 1-4 seconds. GPFA was provoked with eye closure, hyperventilation, and photic stimulation. In all subjects, GPFA was followed by spike-wave discharges (Fig 2). No change in clinical activity is noted during periods of GPFA. Anti-seizure medications had no effect on GPFA. This specific finding was noted during periods of well-controlled epilepsy and absent interictal epileptiform discharges, and on subsequent EEGs recorded 10 years apart. In most subjects, epilepsy was well controlled on one or two anti-seizure medications. Conclusions: GPFA is rare in children with TAS and has marked female preponderance. It is of low voltage and has a posterior predominance. GPFA in TAS is associated with both pharmacoresponsive and drug-resistant epilepsy. It may serve as an independent marker of lifelong epilepsy. Further studies with larger cohort are needed to verify these initial findings. We suggest that children with TAS with the presence of GPFA on their EEG be given the diagnosis “absence epilepsy with GPFA” for more precise identification, prognostication, and better management. Funding: No funding received in support of this abstract/study.
.tmb-.jpg?Culture=en&sfvrsn=7d94e1a1_0)