Electroencephalographic Source Imaging at a Pediatric Epilepsy Center: Physician Impressions After One Year
Abstract number :
1.188
Submission category :
3. Neurophysiology / 3G. Computational Analysis & Modeling of EEG
Year :
2018
Submission ID :
500706
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Matt Lallas, Children's Hospital Los Angeles; Julia Robinson, Children's Hospital Los Angeles; Michele Van Hirtum-Das, Children's Hospital Los Angeles; and Deborah Holder, Children's Hospital Los Angeles
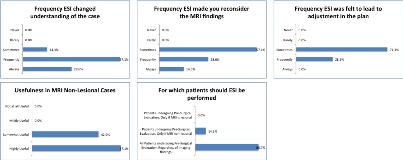
Rationale: Electroencephalographic Source Imaging (ESI) of interictal and ictal epileptiform activity is a validated procedure to help identify the epileptogenic zone from scalp EEG data. Barriers to adopting the technique include lack of familiarity with the processes and with the software, time and experience required to perform the analysis, lack of standardization in the reporting. However, the data obtained may help communicate visually an estimation of the epileptic source. ESI of interictal or occasionally ictal EEG data has been used at the Children’s Hospital Los Angeles since mid-2017 in a limited number of cases using the CURRY 8 software (Compumedics USA, Charlotte, NC). We demonstrate the opinions of the Epilepsy Team after the first year of use of this technology at the CHLA. Methods: As part of a quality assessment, a 7-question survey was sent out to various members of the Epilepsy Team who are typically in attendance at conference, which includes multiple board-certified Epileptologists and Clinical Neurophysiologists, Neuroradiologists, Neurosurgeons, Neuropsychologists, and Epilepsy Fellows. ESI data had previously been presented at conferences when it had been generated. The survey is included in Table 1. Topics of interest were how often the respondents felt the ESI changed their understanding of the case, utility in MRI lesional versus non-lesional cases, and ways to make the data more helpful to the respondents. Results: Seven members of the team responded to the survey. Overall, 6 respondents felt ESI changed their understanding of the patient’s case Frequently or Always. Five felt that the ESI findings Sometimes adjusted the proposed plan. Three felt the findings Frequently or Always made them reconsider the MRI findings while 4 felt that only Sometimes did they reconsider the imaging. All felt ESI was somewhat or highly useful in MRI non-lesional cases, and 6 of the respondents felt ESI should be performed in all patients undergoing Pre-surgical evaluation, regardless of imaging findings. When asked what would make the results more useful, two respondents asked for it to be performed in every case under going pre-surgical evaluation, one asked for further discussion which spikes are being analyzed, one asked that the data be made available earlier to help with imaging interpretation, and one recommended higher electrode count which is already being planned. Conclusions: This survey showed an overall favorable opinion of ESI pre-surgical evaluation of children at our center. Most physicians felt that ESI frequently contributed to better understanding of the patient’s case and planning of the patient’s care. This retrospective assessment of physician opinion is being utilized to drive further improvement in the utilization in this technology at our institution. Future goals include obtaining high-density EEG capability to optimize ESI results, as well as to train technologists and epilepsy fellows to prepare the data in order to reduce the physician time needed. Future prospective quality assessment may also guide growth of this process at CHLA. Funding: No funding was utilized in the generation of this abstract.
.tmb-.jpg?Culture=en&sfvrsn=aaf5dbdb_0)