Evaluation of a Care Coordination Checklist for Pediatric Epilepsy Patients
Abstract number :
1.410
Submission category :
13. Health Services (Delivery of Care, Access to Care, Health Care Models)
Year :
2018
Submission ID :
502501
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Peter Glynn, Nationwide Children's Hospital; Anup D. Patel, Nationwide Children's Hospital; Babitha Harridas, SUNY University at Buffalo; Joanna Seirup, Weill Cornell Medicine; Zula Otgonsuren, Weill Cornell Medicine; and Zachary Grinspan, Weill Cornell M
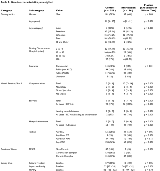
Rationale: Case series data suggests that a care coordination checklist can lead to reduced use of health services for children with epilepsy. A care-coordination checklist is a structured questionnaire that identifies and tracks epilepsy related health problems. However, it is unclear if the observed reductions in use of health services is attributable to the checklist, or if it is part of the natural history of the disease. Methods: We conducted a prospective observational cohort study of a pediatric epilepsy care-coordination checklist at one academic medical center. Enrolled children were identified by clinicians as high risk for frequent emergency department use. We examined outcomes after 1 year. We used propensity score weighting (“weighting by odds”) to compare individuals who received the intervention versus controls. Results: Fifty-six children with epilepsy received the intervention, and 359 did not. Children who received the intervention were younger, were more often male, lived closer to the academic medical center, were more likely to be publicly insured, had more use of health services, were more likely medically complex, were less likely seizure free, and lived in families more impacted by epilepsy, compared to those who did not receive the intervention. Medication side effects were comparable. (Table 1) Within the intervention group after 1 year, median yearly ED visits decreased from 5 [IQI 3–7] to 3 [1–4] (p < 0.001) and unplanned admissions from 2 [0–3] to 1 [0–2] (p = 0.01). There was no change in seizure freedom, impact on family, nor medication side effects. After weighting by the odds to receive the intervention, a weighted control group (effective N = 52.6) was well matched by age, demographics, use of health services, seizure freedom, and impact on family. However, the control group was not well matched on the number of prior ED visits, nor on prior unplanned hospitalizations. (Table 2) The propensity score weighted regression analysis suggested that the intervention had no effect on ED visits (adjusted OR 1.14 [95% CI 0.27 to 4.8]), impact on family scale (0.8 [-1.1 to 2.7] points), medication side effect scale (0.8 [-2.4 to 4.0] points), nor seizure freedom (adjusted OR 1.9 [0.1 to 3.1]). However, there were important differences in unplanned hospitalizations. In the intervention group, the number of individuals with at least one ED visit that lead to an admission dropped from 41 (73%) in the baseline year to 29 (52%) in the second year. In the weighted control group, the number dropped from 22 (41%) to 9 (17%). Thus the risk for unplanned hospitalizations among individuals who received the intervention was increased compared with the weighted control group, even after accounting for the difference in baseline (adjusted OR 4.5 [1.4 to 15]). Conclusions: Children with epilepsy use fewer health services over time. A selected group of children who received a care coordination checklist intervention were subsequently more likely to have unplanned hospitalizations versus matched controls. These findings raise the possibility that active care management may increase use of health services, rather than reduce use. If true, the finding implies an alignment between care management and revenue generation in a fee-for-service reimbursement model, but may be a disincentive to care management in an accountable care organization.However, the analysis was limited by poor matching on ED visits and unplanned hospitalizations. Thus an alternative interpretation is that the checklist was targeted to individuals with a predisposition to have unplanned hospitalizations (i.e., selection bias). Funding: Pediatric Epilepsy Research Foundation
.tmb-.png?Culture=en&sfvrsn=c8389c3d_0)