Mortality in Patients With Psychogenic Non-epileptic Seizures
Abstract number :
1.139
Submission category :
3. Neurophysiology / 3A. Video EEG Epilepsy-Monitoring
Year :
2018
Submission ID :
498473
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Terence J. O’Brien, Central Clinical School, Monash University; Russell Nightscales, University of Melbourne, The Royal Melbourne Hospital; Lara McCartney, University of Melbourne, The Royal Melbourne Hospital; Charles Malpas, University of Melbourn
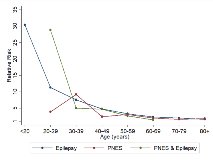
Rationale: Psychogenic non-epileptic seizures (PNES) are a form of conversion disorder that is commonly misdiagnosed and treated as epileptic seizures. People with epilepsy have an elevated risk of death compared with the general population. However, mortality in patients with PNES has received little scientific attention. Methods: In this retrospective cohort study mortality was estimated in patients who had been admitted for a comprehensive epilepsy evaluation to one of two tertiary hospital video EEG monitoring (VEM) units in Melbourne Australia from January 1st 1995 to December 31st 2015. Mortality and cause of death (COD) were determined by linkage to the Australian National Death Index (NDI) and the COD refined based on information from the National Coronial Information System (NCIS) where a coroner’s report was available. Diagnosis was based on the consensus opinion of experienced epileptologists at the Comprehensive Epilepsy Meeting following review of the clinical history, VEM data, and investigations. Mortality was compared in patients classified with PNES, epilepsy or both conditions. Clinical data was extracted by medical record review. Lifetime history of psychiatric disorders was determined from review of neuropsychiatric reports. Results: 3152 patients underwent VEM. 2076 patients were included in the study’s analyses, with 631 diagnosed with PNES, 1339 with epilepsy and 106 with both conditions. The remaining 1076 patients were either non-diagnostic or did not meet the inclusion criteria of the study. Patients diagnosed with PNES have a standardised mortality ratio (SMR) 2.6 times greater than the general population (95% CI 2.0-3.4), with those between the ages of 30 and 39 at 9-fold higher risk of death (95% CI 4.9-17). The SMR of those in the epilepsy group was 3.2 (95% CI = 2.7 – 3.7). There was no significant difference in the rate of mortality between any of the patient groups after excluding epilepsy patients with a known brain tumor at the time of VEM, who had a malignant neoplasm of the brain listed as their primary cause of death (n=17). External causes of death account for 20% (n=10) of all death in those in the PNES group, and 53% (n=8) of deaths with a known cause in those who died below the age of 50. Suicide accounted for 24% (n=4) of deaths in PNES in this age group. Neoplasia and cardiorespiratory causes were responsible for 51% (n=24) of deaths with a known cause across all ages and 67% (n=12) of those aged between 50 and 69. In those with epilepsy external causes accounted for 7% (n=10) of all deaths, whilst neoplasia and cardiorespiratory causes were observed in 42% (n=63) of cases. Epilepsy contributed 28% (n=39) of deaths with a known cause in this group. Conclusions: PNES patients have a SMR over 2.5 times greater than the general population, dying at a rate comparable to those with drug resistant epilepsy. This emphasises the importance of correct diagnosis and identification of relevant pathologies in order to avoid preventable deaths in an important group of patients, where medical attention is often inappropriately directed to dramatic but ultimately irrelevant clinical feature of the condition. Funding: The National Health and Medical Research Council and the RMH Neuroscience Foundation