PATIENT-SPECIFIC SEIZURE ONSET DETECTOR TO OPTIMIZE ICTAL SPECT
Abstract number :
2.188
Submission category :
Year :
2004
Submission ID :
4710
Source :
www.aesnet.org
Presentation date :
12/2/2004 12:00:00 AM
Published date :
Dec 1, 2004, 06:00 AM
Authors :
1Ali Shoeb, 2Blaise Bourgeois, 3Ted Treves, and 4John Guttag
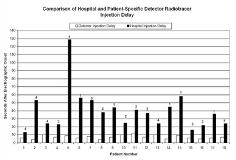
Prompt administration of radiotracers following the [italic]electrographic onset[/italic] of a seizure may enhance the localization of epileptogenic foci using functional imaging modalities such as SPECT. In our experience, ictal SPECT protocols that rely on a caregiver for visual recognition of a seizure[apos]s onset result in injection of the radiotracer 20-55 seconds after the [italic]clinical onset[/italic]. This delay leads to poor localization of the seizure focus. To achieve consistent and prompt injection of radiotracers we developed an automated patient-specific method for the detection of seizure onsets from non-invasive EEG. The detector can alert staff of a seizure[apos]s electrical onset, or automatically activate a drug infusion pump that delivers the radiotracer. Our [italic]patient-specific[/italic] detector exploits the consistency of seizure and non-seizure EEG within patients. The detector uses a wavelet decomposition to construct a feature vector that captures the morphology and spatial distribution of waveforms in a 2 second EEG epoch. Next, the detector determines whether that feature vector is representative of a patient[apos]s seizure or non-seizure EEG using a classifier (a support-vector machine) that has already been trained to recognize that patient[apos]s seizure and non-seizure activity. When the detector notes seizure activity for six seconds it declares a seizure event. The detector was tested on EEG from forty-six pediatric subjects. It detected 160 of 168 seizure events within 7.9 +/- 3.0 seconds following the electrographic onset, and declared 22 false-detections in 75 hours of clinical EEG. The figure below compares the delay incurred by starting injection of the radiotracer using existing hospital protocols with the delay that would be incurred provided injections were triggered by the detector. The numbers over each bar indicate how many seizures the detector was trained on before attempting to detect the seizure on which an ictal SPECT was attempted.[figure1] We have developed a patient-specific method that detects the onset of epileptic seizures from non-invasive EEG. That method is well suited for triggering time-sensitive clinical procedures like injection of a radiotracer following seizure onset for the purpose of seizure focus localization. (Supported by Center for Integration of Medicine and Innovative Technology (CIMIT) and the MIT Project Oxygen Partnership.)