Periodic and Rhythmic EEG Patterns: Is There Clinical Equipoise for Treatment in Hospitalized Patients?
Abstract number :
2.027
Submission category :
3. Neurophysiology / 3B. ICU EEG
Year :
2018
Submission ID :
502584
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Daniela R. Galluzzo, Yale University School of Medicine; Monica Dhakar, Emory University School of Medicine; Lawrence J. Hirsch, Yale University School of Medicine; Kevin N. Sheth, Yale University School of Medicine; and Emily J. Gilmore, Yale University
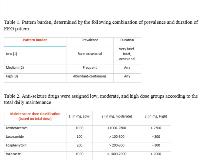
Rationale: Increased availability and use of cEEG monitoring in hospitalized patients has led to the identification of periodic and rhythmic patterns, the spectrum of which have unclear clinical significance. Resultantly, the degree and aggressiveness to which these patterns warrant treatment remains uncertain. We present our single center’s pragmatic experience in the treatment of lateralized periodic discharges (LPDs), lateralized rhythmic delta activity (LRDA), and generalized periodic discharges (GPDs). Methods: As part of a prospective observational study of patients on the ictal-interictal continuum who were enrolled after being loaded with an antiseizure drug (ASD), we retrospectively reviewed excluded patients’ charts (N=358) for various clinical, pharmacologic, EEG, imaging and outcome variables. Pattern burden was scored (1, 2, and 3) according to the combination of prevalence and duration of EEG pattern (‘burden’) described in Table 1. ASDs were assigned low, moderate, and high dose groups according to the total daily maintenance dose described in table 2. Results: The average age was 65 years (16-98), with 45% being male. Two hundred eighty-three (79%) of these patients were admitted for neurologic conditions, with ischemic and hemorrhagic stroke (37%) being the most common etiology. Clinical seizures prior to cEEG were reported in 106 (46%). Sixty-six (18%) patients had a prior history of epilepsy. Magnetic resonance imaging was performed in 253 (71%), with abnormal MRI findings in 223 (88%). Abnormalities were focal in 156 (69%), and diffuse in 69 (31%). Three hundred seven patients (86%) were evaluated with cEEG to rule out the presence of non-convulsive seizures or status epilepticus. Two hundred twenty-eight (64%) exhibited altered mental status during cEEG monitoring. The predominant cEEG patterns in the first 24 hours were LRDA (149; 42%)), LPDs (130; 36%), and GPDs (79; 22%). Patients were monitored for an average of 42 hours (±20). Fifty-nine (16%) patients were not started on an anti-seizure drug (ASD). Of the 294 patients on an ASD, 74 (25%) had an electrographic seizure, sixty-six (89%) of which were on a moderate-high dose ASD. Sixty-two (50%) patients with a low pattern burden on cEEG were either placed on a low dose ASD or none at all, compared to 20 (23%) patients with a high pattern burden. Of those who were not treated at all, none had electrographic seizures for the remainder of their monitoring. One hundred thirty-seven (68%) of patients with a frequent, abundant, or continuous pattern prevalence were started on a moderate-high dose ASD and were more likely to be on an ASD at discharge and follow-up. Conclusions: Future trials are needed to address if, to what degree, and for how long hospitalized patients with IIC patterns should be managed with ASDs. A low pattern burden may not warrant treatment; preliminary data suggests that patients who were not treated did not have any electrographic seizures on subsequent days of monitoring. Additionally, we may be over treating patients with low frequency patterns, suggesting that there may be clinical equipoise regarding the decision and aggressiveness to which rhythmic and periodic patterns with a low to moderate burden are treated. Funding: American Brain Foundation/American Academy of Neurology