Predictors of Healthcare Transition Readiness in Adolescents and Young Adults with Epilepsy
Abstract number :
2.358
Submission category :
11. Behavior/Neuropsychology/Language / 11B. Pediatrics
Year :
2018
Submission ID :
502076
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Aimee W. Smith, Cincinnati Children's Hospital Medical Center; Ana Gutierrez-Colina, Cincinnati Children's Hospital Medical Center; Emily Roemisch, Cincinnati Children's Hospital Medical Center; Brooke Hater, Cincinnati Children's Hospital Medical Center;
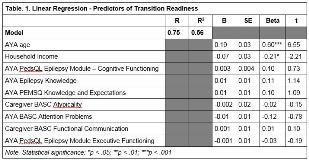
Rationale: Adolescents and young adults (AYAs) with epilepsy may need to transition from pediatric to adult healthcare settings. Unfortunately, the transition process is a vulnerable period that can lead to discontinuity of care, decreased quality of life, treatment non-adherence, and excess morbidity. Therefore, it is critical to evaluate the processes and factors that impede or promote transition. The social-ecological model of AYA readiness for transition (SMART) can be used to guide such evaluations. The aims of the current study are to 1) characterize transition readiness in AYAs with epilepsy, and 2) validate the SMART model in a sample of AYAs with epilepsy. It was hypothesized that 1) AYAs in the current study would demonstrate variable rates of transition readiness, and 2) socioecological factors conceptualized by the SMART model as modifiable and non-modifiable would be significantly related to transition readiness in AYAs with epilepsy. Methods: Participants included youth with epilepsy 13-25 years of age seen in a comprehensive epilepsy center. This cross sectional study assessed AYA-report of transition readiness (Transition Readiness Assessment Questionnaire; TRAQ), epilepsy knowledge, epilepsy self-management, developmental factors and emotional and behavioral functioning. AYAs and healthcare providers also completed a measure of their relationship quality. Caregiver report was included when available. Results: Participants included 82 AYAs (M=17.3+2.8; 86.6% White Non-Hispanic, 53.7% females) with epilepsy. TRAQ scores (X=3.33, SD=0.86) were significantly correlated with modifiable and non-modifiable factors: age (r=0.66, p<.001), income (r=-0.23, p=.04), AYA cognitive problems (r=0.24, p=0.03), AYA knowledge (r=0.31, p<.01), AYA expectations (r=0.26, p<.05), AYA inattention (r=-0.24, p<.05), AYA executive dysfunction (r=0.25, p<.05), caregiver-reported AYA odd behaviors (r=-0.25, p<.05), and caregiver-reported AYA communication problems (r=0.25, p<.05). TRAQ scores were not related to other demographic (e.g., minority status, insurance), medical (years since diagnosis, type of epilepsy, polytherapy, seizure frequency), developmental factors (e.g., adaptive skills, cognitive functioning) or emotional/behavioral factors (e.g., skills, relationship with provider, psychosocial functioning). Linear regression including variables significantly correlated with the outcome of transition readiness (F (9, 60) = 8.32, p < .001) explained 56% of variance. Specifically, age and income were significant model predictors (see Table 1). Conclusions: Overall, AYAs with epilepsy displayed a level of transition readiness similar to previously-reported scores in healthcare settings. Age and income, but not other theoretically-hypothesized factors, predicted transition readiness in AYAs with epilepsy. More work is needed to identify potential targets of intervention to improve transition readiness in AYAs with epilepsy. Additionally, given the generic nature of our measure of transition readiness (TRAQ), aspects of epilepsy-specific transition readiness that are more salient to our population may not have been captured. Future research should example a competency-based model of care and consider using an epilepsy-specific measure of transition readiness. Funding: This work was supported by the Endowed Scholars Award through Cincinnati Children’s Hospital Center, awarded to Avani C. Modi.