Retinal Structure and Function in Adults with Refractory Complex Partial Seizures (rCPS) Treated with Vigabatrin: Initial Results of the Sabril Vision Study
Abstract number :
3.302
Submission category :
Late Breakers
Year :
2013
Submission ID :
1860137
Source :
www.aesnet.org
Presentation date :
12/7/2013 12:00:00 AM
Published date :
Dec 5, 2013, 06:00 AM
Authors :
C. A. Johnson, R. Sergott, K. Laxer, R. Wechsler, Y. Dribinsky, C. Canavan, J. Isojarvi, D. Lee
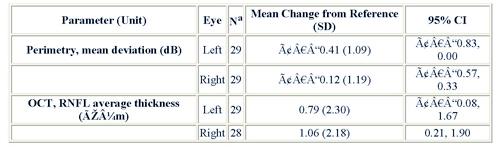
Rationale: Bilateral concentric constriction of peripheral visual fields has been reported for 30 40% of those receiving vigabatrin (VGB). However, these data arise from cross-sectional studies without baseline values. Results from the Sabril Registry1, Gonzalez et al.2, and Sergott et al.3 indicate >20% of patients have pre-existing afferent visual system abnormalities at baseline, which has not been accounted for in previous VGB studies. To define changes in optic nerve and retinal structure and function, we are conducting an ongoing, prospective, 1-year, open-label trial of VGB as adjunctive therapy for adults with rCPS. We report interim results for the first 30 patients to reach their first post-reference vision assessments (3 months).Methods: Planned enrollment is ~80 VGB-na ve patients 18 years of age with rCPS for 1 year at ~25 US sites.4 Patients must have had 2 seizures/month averaged over prior 3 months, must have failed 3 prior therapies for lack of efficacy, and must be receiving concomitant AEDs.4 Patients must be able to perform static perimetry and spectral optical coherence tomography (OCT) in a reliable, reproducible manner at reference (baseline, 0 26 days, and 2 28 days), and 3, 6, 9, and 12 months following VGB initiation.4 Key endpoints include changes from reference values in visual fields, and in retinal nerve fiber layer (RNFL) and macular thickness by OCT. Central readers at 2 vision research centers review de-identified visual field and OCT reports. If deficits are discovered, investigators conduct benefit/risk assessments with patients.4Results: By May 16, 2013, 56 patients had been screened at 19 sites, and 38 had been enrolled and treated. 17 patients were screen failures, 12 of whom could not complete perimetry or OCT assessments within the allotted time. (1 patient had not yet been treated.) Of the 38 treated, 24 were ongoing, 9 were early terminations, and 5 had completed the study. Mean age was 39.3 years (19.0 69.0 years), and 61% were male. Comorbidities included history of ophthalmic issues (18%), psychiatric disorders (68%), cognitive impairment (20%), and surgery to treat seizures (66%). 25 of 60 eyes (42%) evaluated (30 patients) had abnormal OCT findings at baseline, and 20 of these 25 eyes (80%) with abnormal OCT findings also had thin RNFLs. Interim vision findings are provided (table). 3 patients (7.9%) had SAEs, and the most common AEs were convulsion (18.4%) and falls (10%). 3 patients (7.9%) had AEs of blurry vision.Conclusions: This interim analysis suggests underlying conditions and prior therapies may affect vision and vision testing. Based on perimetry, there did not appear to be clinically relevant worsening of central visual fields. OCT findings demonstrated RNFL thickening in some of these first 30 patients to reach 3 months of therapy. 1Sergott R, et al. AES 2012 Late-Breaking Abstract #1.369. 2Gonzalez P, et al. Epilepsy Behav. 2009;16:521 6. 3Sergott R, et al. Epilepsy Res. 2010;92:170 6. 4Sergott R, et al. Epilepsy Curr. 2011;11(1 Suppl 1):Abstract #1.294.